Legends Of Respiratory Care

Legends of Respiratory Care
The designation as a Legend of Respiratory Care is an honor bestowed upon an individual who significantly impacted and changed the respiratory care profession.


What is a Legend of Respiratory Care?
The designation as a Legend of Respiratory Care is an honor bestowed upon an individual who changed the respiratory care profession through:
* Scientific achievements and/or inventions of historical significance that revolutionized, or remarkably enhanced the delivery of respiratory care;
* Recognized professional achievements related to the clinical practice, education, or the science of respiratory care, publication of scientific articles or other activities bringing significant, sustained career recognition;
* Sustained personal service, representation, or advocacy on behalf of the respiratory care profession, and/or individual’s creativity or ideas that resulted in historic advancement of the profession or its professional societies; and
* Singularly distinctive individual actions during historic professional events, above and beyond reasonable expectations, that resulted in advancement of respiratory care and/or resolution of a significant crisis or issue facing the profession.
Nominations are solicited from the AARC, ARCF, CoARC and NBRC. Nominations must be supported by two-thirds of the agency’s governing board. After receipt of the combined roster of nominees, a review committee elects the requisite number of Legends of Respiratory Care.
* Scientific achievements and/or inventions of historical significance that revolutionized, or remarkably enhanced the delivery of respiratory care;
* Recognized professional achievements related to the clinical practice, education, or the science of respiratory care, publication of scientific articles or other activities bringing significant, sustained career recognition;
* Sustained personal service, representation, or advocacy on behalf of the respiratory care profession, and/or individual’s creativity or ideas that resulted in historic advancement of the profession or its professional societies; and
* Singularly distinctive individual actions during historic professional events, above and beyond reasonable expectations, that resulted in advancement of respiratory care and/or resolution of a significant crisis or issue facing the profession.
Nominations are solicited from the AARC, ARCF, CoARC and NBRC. Nominations must be supported by two-thirds of the agency’s governing board. After receipt of the combined roster of nominees, a review committee elects the requisite number of Legends of Respiratory Care.


2014 Legends of Respiratory Care
In the inaugural year of the program, ten individuals were selected as Legends.
Vivian Ray Bennett
Vivian Ray Bennett, was an inventor who developed a gas delivery system that incorporated a jeweled pneumatic valve. Bennett received multiple patents for his ventilator components and patient connection devices. His patented valve was first incorporated in a Bennett Pressure Breathing Unit in 1948 and utilized in early respiration units including the TV2P, PR-1, PR-2, AP-4, and AP-5.
Bennett founded V. Ray Bennett and Associates Ventilator Company in Santa Monica CA in the early 1940s. His valve and early ventilator devices were initially used in the treatment of polio in southern California and significantly improved the survival of polio patients compared to polio patients ventilated in iron lungs.
In 1957, the Puritan Company acquired V. Ray Bennett and Associates Ventilator Company and emerged as Puritan Bennett Respiration Products, Inc.
Bennett founded V. Ray Bennett and Associates Ventilator Company in Santa Monica CA in the early 1940s. His valve and early ventilator devices were initially used in the treatment of polio in southern California and significantly improved the survival of polio patients compared to polio patients ventilated in iron lungs.
In 1957, the Puritan Company acquired V. Ray Bennett and Associates Ventilator Company and emerged as Puritan Bennett Respiration Products, Inc.
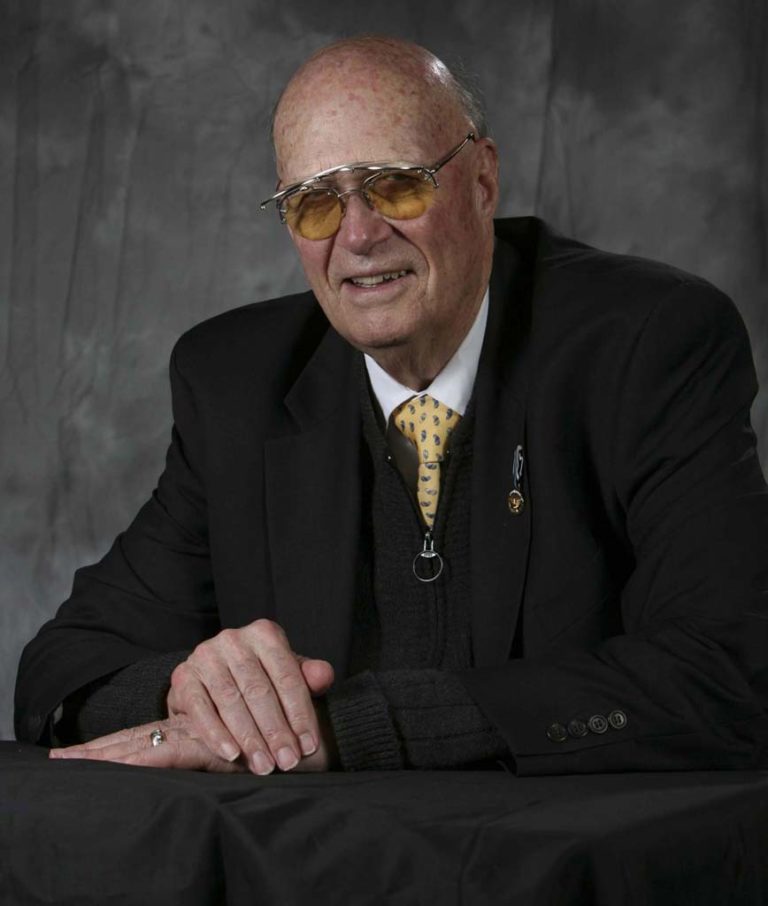

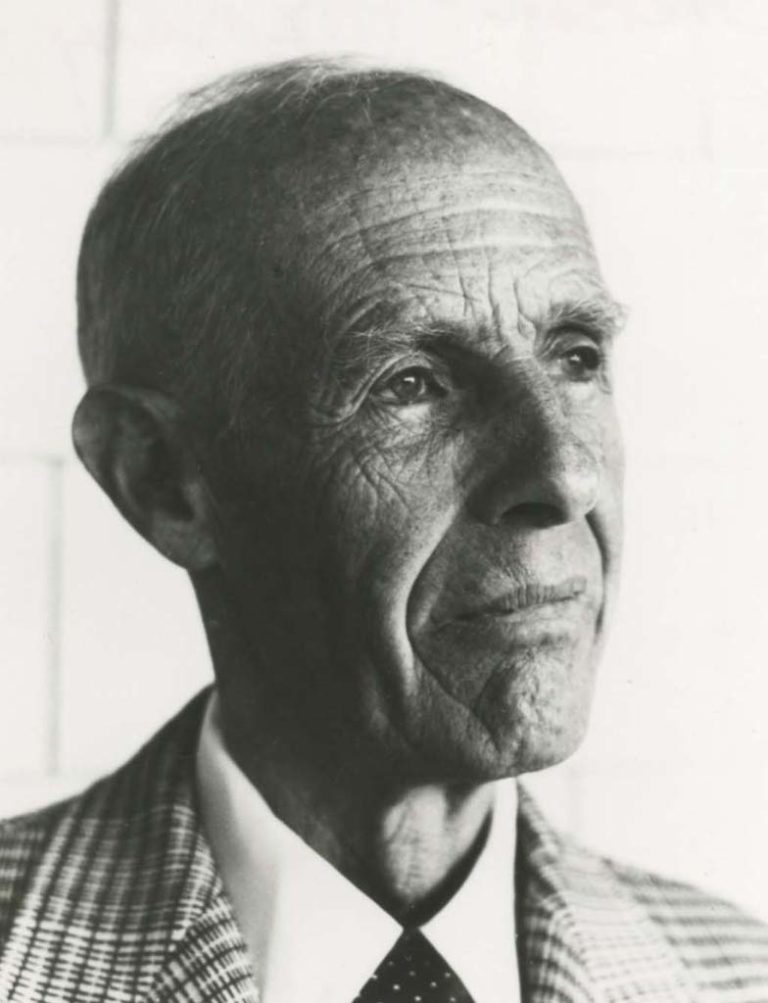
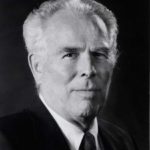
Forrest M. Bird, PhD, MD, FAARC
Forrest M. Bird, PhD, MD was an aviator, inventor, scientist, and biomedical engineer.
Following his service in the Army Air Corps where he was a technical air training officer, Forrest Bird earned his medical degree and began developing a number of medical devices. In 1955, he developed the Bird Universal Medical Respirator. A number of Bird ventilators were introduced including the Babybird respirator in1969.
Dr. Bird was a recipient of the Jimmy A. Young Medal, the AARC’s highest honor.
President George W. Bush presented Dr. Bird the Presidential Citizens Medal in December 2008. President Barach Obama presented Dr. Bird the National Medal of Science and Technology, the nation’s highest honor for science and technology in October 2009.
Following his service in the Army Air Corps where he was a technical air training officer, Forrest Bird earned his medical degree and began developing a number of medical devices. In 1955, he developed the Bird Universal Medical Respirator. A number of Bird ventilators were introduced including the Babybird respirator in1969.
Dr. Bird was a recipient of the Jimmy A. Young Medal, the AARC’s highest honor.
President George W. Bush presented Dr. Bird the Presidential Citizens Medal in December 2008. President Barach Obama presented Dr. Bird the National Medal of Science and Technology, the nation’s highest honor for science and technology in October 2009.

Donald F. Egan, MD
Donald Francis Egan, MD served as the first Medical Director of the Inhalation Therapy Department at Yale University. He helped establish one of the first inhalation therapy schools in the country. In 1968 he relocated to Connecticut to head the Pulmonary Disease Department at New Britain General Hospital.
Dr. Egan authored the first comprehensive textbook on inhalation therapy. Fundamentals of Inhalation Therapy was published by Mosby in 1969. It contained 474 pages. Egan’s Fundamentals of Respiratory Care, a standard textbook in most respiratory care programs, is now in its 10th edition.
Dr. Egan authored the first comprehensive textbook on inhalation therapy. Fundamentals of Inhalation Therapy was published by Mosby in 1969. It contained 474 pages. Egan’s Fundamentals of Respiratory Care, a standard textbook in most respiratory care programs, is now in its 10th edition.
John Haven "Jack" Emerson
Although this self-taught inventor never completed high school, J.H. “Jack” Emerson’s creativity and inventive designs resulted in 35 US patents for biomedical devices and diving equipment.
Emerson invented major modifications to the iron lung respirator and added important safety features. A patent dispute with Drinker resulted. (Not only did Drinker lose the lawsuit, Drinker’s patent for the iron lung respirator was rescinded.) Emerson’s original iron lung,” Old Number One,” is displayed in the National Museum of American History of the Smithsonian in Washington, D.C.
Emerson invented major modifications to the iron lung respirator and added important safety features. A patent dispute with Drinker resulted. (Not only did Drinker lose the lawsuit, Drinker’s patent for the iron lung respirator was rescinded.) Emerson’s original iron lung,” Old Number One,” is displayed in the National Museum of American History of the Smithsonian in Washington, D.C.


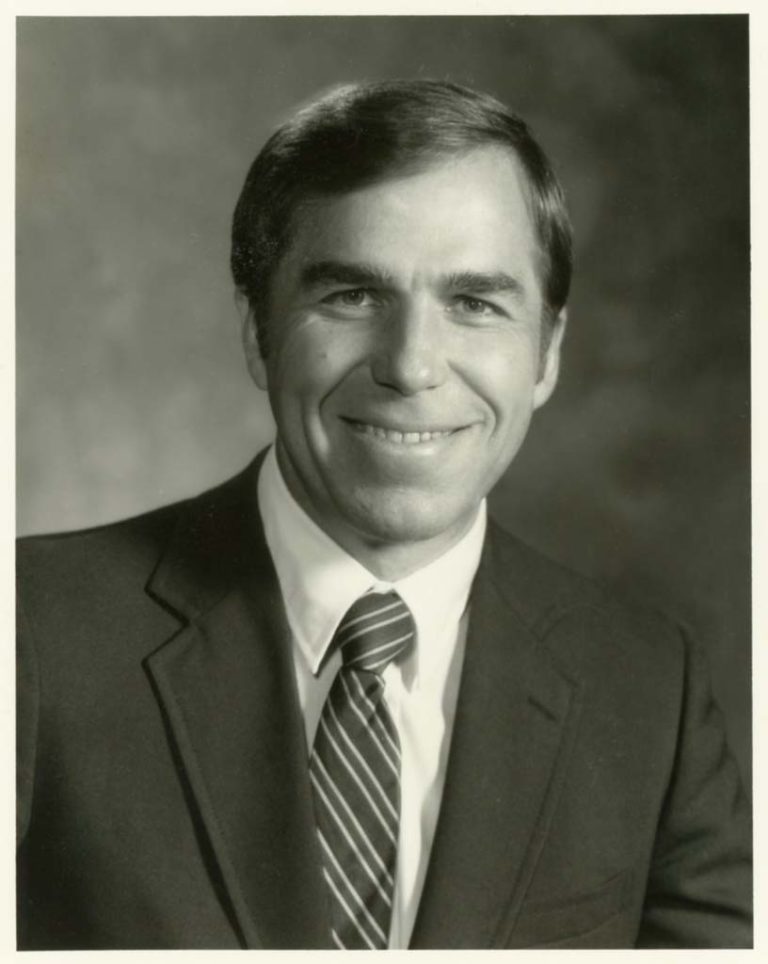
Sam P. Giordano, MBA, RRT, FAARC
Sam Giordano, MBA, RRT, FAARC Giordano joined the AAIT in 1964. He served as President in 1980. In 1981, Giordano was hired as Executive Director of the AARC, a position he held until his retirement in 2012.
Giordano was a true visionary for the Association and the respiratory care profession and was instrumental in leading the AARC into the international arena.
Among the numerous awards Giordano has received are the Jimmy A.Young Medal, the highest honor awarded by the AARC and the Héctor León Garza Achievement Award for Excellence in International Respiratory Care.
Giordano was a true visionary for the Association and the respiratory care profession and was instrumental in leading the AARC into the international arena.
Among the numerous awards Giordano has received are the Jimmy A.Young Medal, the highest honor awarded by the AARC and the Héctor León Garza Achievement Award for Excellence in International Respiratory Care.
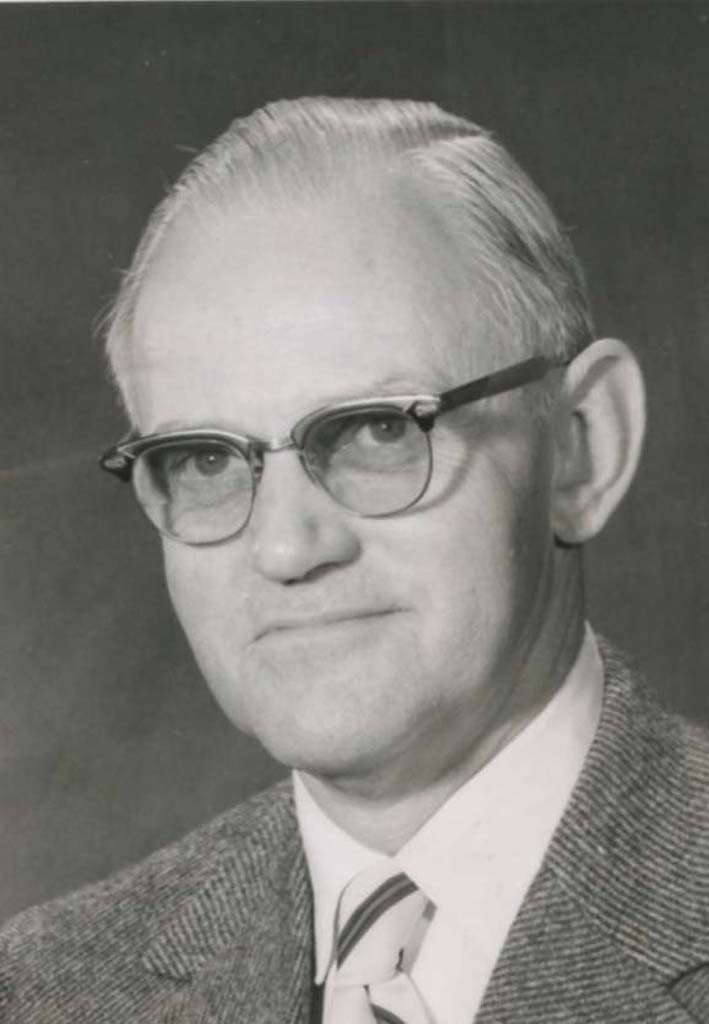
Henry Frederic Helmholz, Jr. MD
H. Fred Helmholz, Jr. MD was a graduate of John Hopkins University School of Medicine in 1937. Dr. Helmholz was a researcher in circulatory and respiratory physiology at Mayo Clinic in Rochester, Minnesota from 1943-1967. He served as the Medical Director of Inhalation Therapy at Mayo Clinic.
Dr. Helmholz was actively involved in all aspects of the respiratory care profession: accreditation, credentialing, and education. Dr. Helmholz was a recipient of the Jimmy A. Young Medal, the highest honor awarded by the AARC. Dr. Helmholz was a published poet and a beloved, long-time judge of the AARC’s Sputum Bowl.
Dr. Helmholz was actively involved in all aspects of the respiratory care profession: accreditation, credentialing, and education. Dr. Helmholz was a recipient of the Jimmy A. Young Medal, the highest honor awarded by the AARC. Dr. Helmholz was a published poet and a beloved, long-time judge of the AARC’s Sputum Bowl.
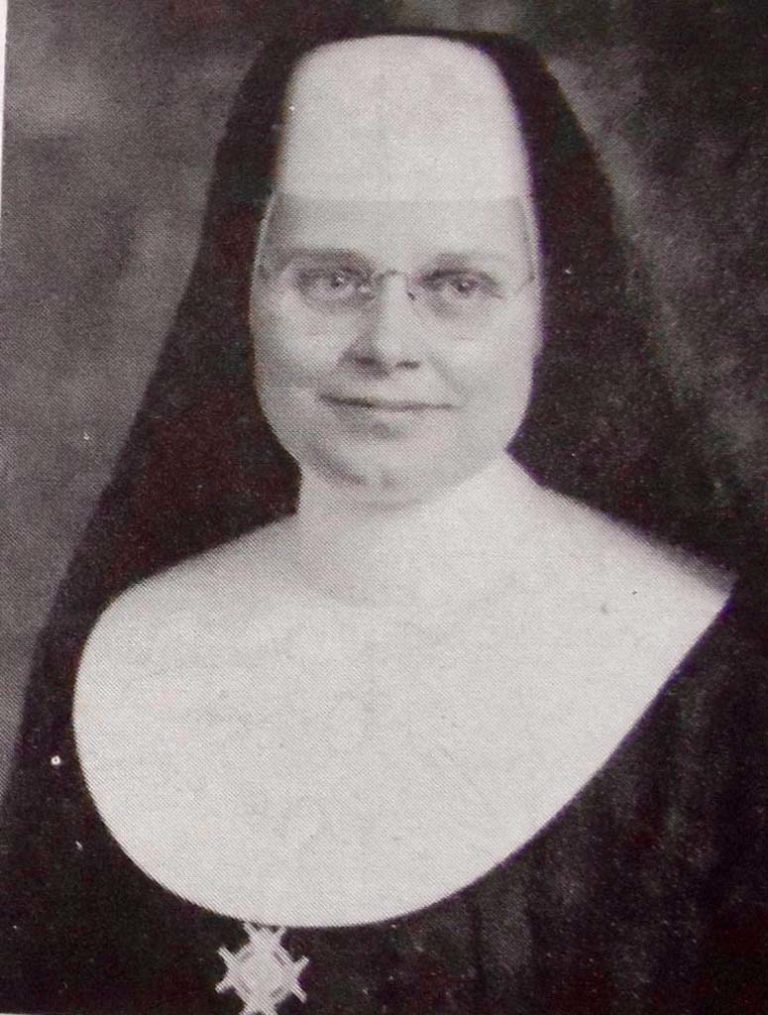

Sr. M. Yvonne Jenn, BS, RN, ARIT
Sister M. Yvonne Jenn was one of the nine incorporators of the American Registry of Inhalation Therapists (now NBRC). In November 1960, Sister M. Yvonne Jenn became the first Registered Inhalation Therapist in the USA.
She was a CRNA and served as a program director of the Franciscan Skemp School of Nurse Anesthesia in La Crosse, WI. Sister Yvonne served on the AAIT Board of Directors and served as Executive Director of the American Registry of Inhalation Therapists. The NBRC’s highest award in named in her honor: the Sister Mary Yvonne Jenn, CRNA, RRT Lifetime Achievement Award.
She was a CRNA and served as a program director of the Franciscan Skemp School of Nurse Anesthesia in La Crosse, WI. Sister Yvonne served on the AAIT Board of Directors and served as Executive Director of the American Registry of Inhalation Therapists. The NBRC’s highest award in named in her honor: the Sister Mary Yvonne Jenn, CRNA, RRT Lifetime Achievement Award.


Brother Roland Maher
In 1947, Brother Roland Maher was one of the five incorporators of the Inhalation Therapy Association (now AARC).
Brother Maher was the first person to serve as Assistant Chairman (now Vice-President) of the ITA and served multiple elected terms as President of the Association:1949-1951 and 1953-1954. Brother Maher received the Jimmy A. Young Medal, the highest honor awarded by the AARC.
Brother Maher was the first person to serve as Assistant Chairman (now Vice-President) of the ITA and served multiple elected terms as President of the Association:1949-1951 and 1953-1954. Brother Maher received the Jimmy A. Young Medal, the highest honor awarded by the AARC.


George A. Kneeland
George A. Kneeland was one of the five incorporators of the Inhalation Therapy Association (now AARC) in 1947.
He was the first to hold the office of Chairman (now President) of the ITA in 1947-1948. Kneeland received the Jimmy A. Young Medal, the highest honor awarded by the AARC.
He was the first to hold the office of Chairman (now President) of the ITA in 1947-1948. Kneeland received the Jimmy A. Young Medal, the highest honor awarded by the AARC.


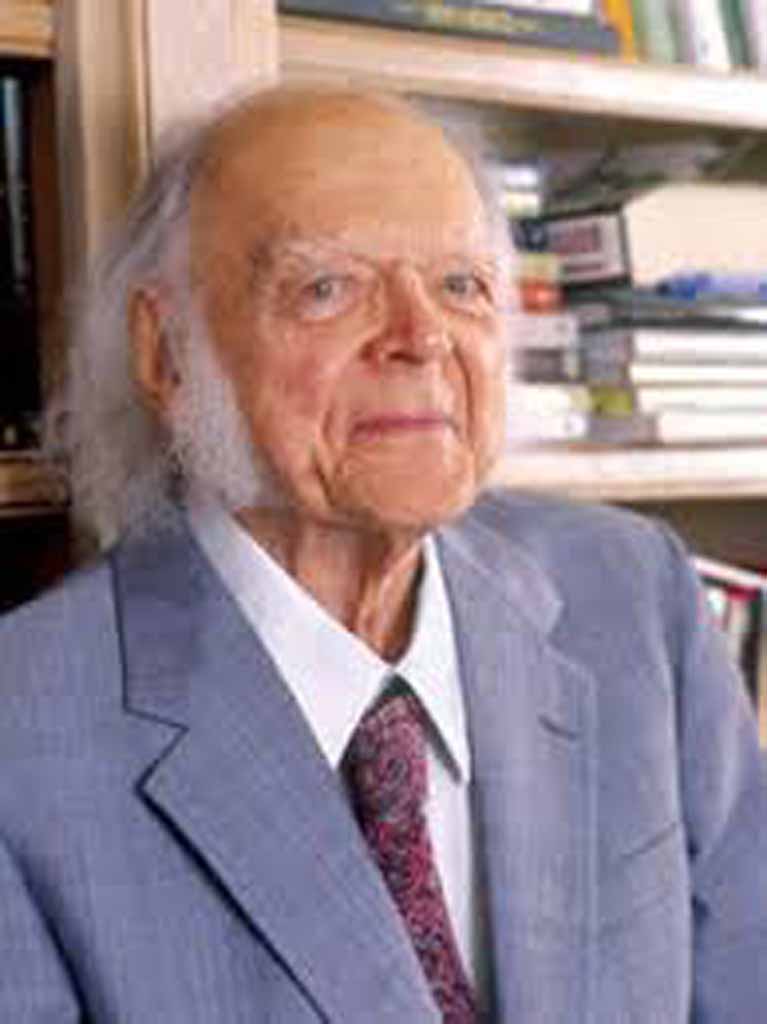
Thomas L. Petty, MD, FAARC
Thomas L. Petty, MD was a pulmonologist who published over 800 journal articles in journals and authored or edited over 45 books or editions.
Dr. Petty was Professor Emeritus of Medicine at the University of Colorado Health Sciences Center in Denver and Emeritus Professor of Medicine at National Jewish Medical & Research Center.
Dr. Petty and his colleagues were among the first to research ARDS and the first to use PEEP in its treatment. He also was instrumental in using long-term home oxygen therapy for the management of COPD and for demonstrating the benefits of pulmonary rehabilitation programs. He was a true patient advocate and answered questions from patients in Ask Dr. Tom on the AARC’s Your Lung Health website.
Dr. Petty was recognized as a FAARC in 1999. He was a recipient of the Jimmy A. Young Medal, the highest honor awarded by the AARC.
Dr. Petty was Professor Emeritus of Medicine at the University of Colorado Health Sciences Center in Denver and Emeritus Professor of Medicine at National Jewish Medical & Research Center.
Dr. Petty and his colleagues were among the first to research ARDS and the first to use PEEP in its treatment. He also was instrumental in using long-term home oxygen therapy for the management of COPD and for demonstrating the benefits of pulmonary rehabilitation programs. He was a true patient advocate and answered questions from patients in Ask Dr. Tom on the AARC’s Your Lung Health website.
Dr. Petty was recognized as a FAARC in 1999. He was a recipient of the Jimmy A. Young Medal, the highest honor awarded by the AARC.


Two of the Greats
Dr. Fred Helmholz and Dr. Forrest Bird, two of our Legends, are shown in this photo taken at an event held at Mayo Clinic in Rochester Minnesota.
Tom Kallstrom


2015 Legends of Respiratory Care
Five individuals were selected as the 2015 Legends of Respiratory Care.

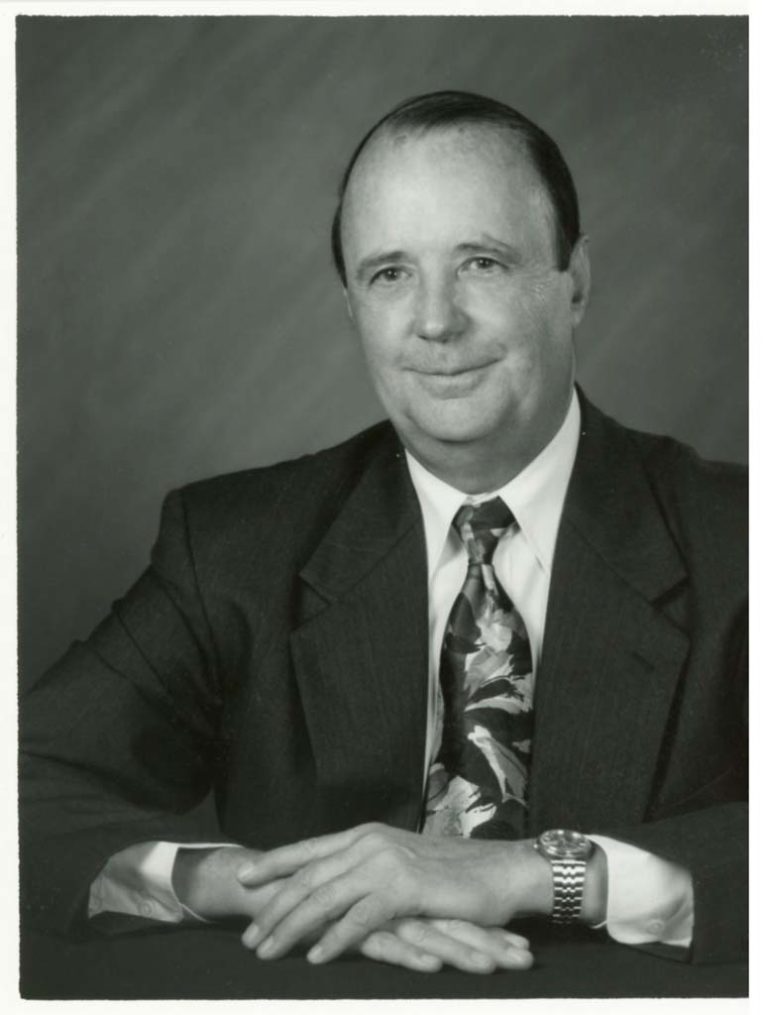
George G. Burton, MD, FAARC
Dr. George Burton has been actively involved in respiratory care and pulmonary medicine since he began his clinical practice in Pulmonary Disease at Loma Linda University in 1967. He has held prominent positions at several hospitals in Southern California, and has been affiliated with Kettering Medical Center in Dayton OH since 1983, serving as Medical Director for Respiratory Care Services from 1983 to 2001, and as Medical Director for their Sleep Disorder Center from 1985 to the present.
Dr. Burton’s major contributions to respiratory care have been in the educational arena through his writings and service related to accreditation of respiratory care programs as evidenced by his participation with the Commission on Accreditation for Respiratory Care (CoARC), its predecessor, the Joint Review Committee for Respiratory Therapy Education (JRCRTE) and the Commission on Accreditation of Allied Health Education Programs (CAAHEP).
Dr. Burton co-authored a comprehensive textbook for respiratory care students in 1977. This book quickly became a required text for programs, and literally thousands of students learned the essential aspects of the practice of respiratory care by reading and implementing the recommendations offered in the three editions of this text. He then turned his attention to promoting Respiratory Therapist Driven Protocols in two textbooks authored in conjunction with Judy Tietsort. Dr. Burton’s most recent writings have been the Clinical Manifestations of Respiratory Disease with Terry Des Jardins. This text was first introduced in 1994 and is now in its seventh edition.
In his role as Medical Director for the Respiratory Care Program at Kettering College in Dayton OH for 33 years, Dr. Burton has participated directly in the education of hundreds of respiratory therapist. He has participated in probably 400 student case study presentations. He also serves as a mentor for the faculty at Kettering College, many of whom have gone on to serve in leadership positions with the AARC, CoARC, and their organizations.
Service to program accreditation continues to be a passion of Dr. Burton. His active participation with the JRCRTE began in 1976 as an ACCP representative. Since that time, he has chaired subcommittees for Standards Revisions, participated in many Site Visits, and participated in the transition from the JRCRTE to CoARC. Today he remains active as a member of CoARC’s Post Professional Education Committee. He also served on the Board of Directors of the Commission on Accreditation of Allied Health Education Programs (CAAHEP).
Dr. Burton’s major contributions to respiratory care have been in the educational arena through his writings and service related to accreditation of respiratory care programs as evidenced by his participation with the Commission on Accreditation for Respiratory Care (CoARC), its predecessor, the Joint Review Committee for Respiratory Therapy Education (JRCRTE) and the Commission on Accreditation of Allied Health Education Programs (CAAHEP).
Dr. Burton co-authored a comprehensive textbook for respiratory care students in 1977. This book quickly became a required text for programs, and literally thousands of students learned the essential aspects of the practice of respiratory care by reading and implementing the recommendations offered in the three editions of this text. He then turned his attention to promoting Respiratory Therapist Driven Protocols in two textbooks authored in conjunction with Judy Tietsort. Dr. Burton’s most recent writings have been the Clinical Manifestations of Respiratory Disease with Terry Des Jardins. This text was first introduced in 1994 and is now in its seventh edition.
In his role as Medical Director for the Respiratory Care Program at Kettering College in Dayton OH for 33 years, Dr. Burton has participated directly in the education of hundreds of respiratory therapist. He has participated in probably 400 student case study presentations. He also serves as a mentor for the faculty at Kettering College, many of whom have gone on to serve in leadership positions with the AARC, CoARC, and their organizations.
Service to program accreditation continues to be a passion of Dr. Burton. His active participation with the JRCRTE began in 1976 as an ACCP representative. Since that time, he has chaired subcommittees for Standards Revisions, participated in many Site Visits, and participated in the transition from the JRCRTE to CoARC. Today he remains active as a member of CoARC’s Post Professional Education Committee. He also served on the Board of Directors of the Commission on Accreditation of Allied Health Education Programs (CAAHEP).


Robert Lawrence, MD
Dr. Lawrence first became involved with respiratory therapy in 1958. He served on the AARC’s Board of Medical Advisors in 1964, and the organization’s Technician Certification Board in 1968 and 1969. These activities cemented his amorous affair with respiratory therapy and set the stage for greater contributions as the future of the profession unfolded.
Dr. Lawrence took over the RRT Oral Examinations in 1969. He worked tirelessly from his home office to “give the RRT Oral Examinations back to the candidates”. From 1969 through 1978, he scheduled thousands of oral examination sessions for candidates and was a staunch candidate advocate. All examiners were well familiar with the Pre-Exam meeting the evening before the exams began the next morning. His instructions were simple, "This is the candidate's exam and if that's not your purpose for being here, you may go back home with my blessings". He was true to his word and removed examiners for failing to follow those instructions. He served as the Executive Secretary of the NBRC in 1969 and charged $1 per year, compensation he never accepted. Thus, he was the second chief executive of what is now the NBRC.
Dr. Lawrence’s service to the profession and the credentialing system continued with his appointment to the NBRC as a trustee from 1974 through 1986 as a representative of the American Society for Anesthesiologists (ASA). He was elected by his colleagues on the NBRC to serve as the organization’s President in 1985. His contributions to respiratory therapy were witnessed by several generations and will never be forgotten.
Dr. Lawrence took over the RRT Oral Examinations in 1969. He worked tirelessly from his home office to “give the RRT Oral Examinations back to the candidates”. From 1969 through 1978, he scheduled thousands of oral examination sessions for candidates and was a staunch candidate advocate. All examiners were well familiar with the Pre-Exam meeting the evening before the exams began the next morning. His instructions were simple, "This is the candidate's exam and if that's not your purpose for being here, you may go back home with my blessings". He was true to his word and removed examiners for failing to follow those instructions. He served as the Executive Secretary of the NBRC in 1969 and charged $1 per year, compensation he never accepted. Thus, he was the second chief executive of what is now the NBRC.
Dr. Lawrence’s service to the profession and the credentialing system continued with his appointment to the NBRC as a trustee from 1974 through 1986 as a representative of the American Society for Anesthesiologists (ASA). He was elected by his colleagues on the NBRC to serve as the organization’s President in 1985. His contributions to respiratory therapy were witnessed by several generations and will never be forgotten.
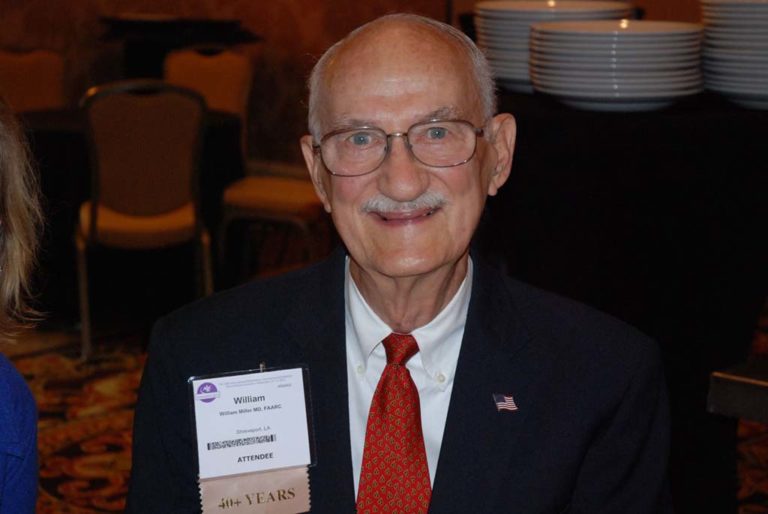

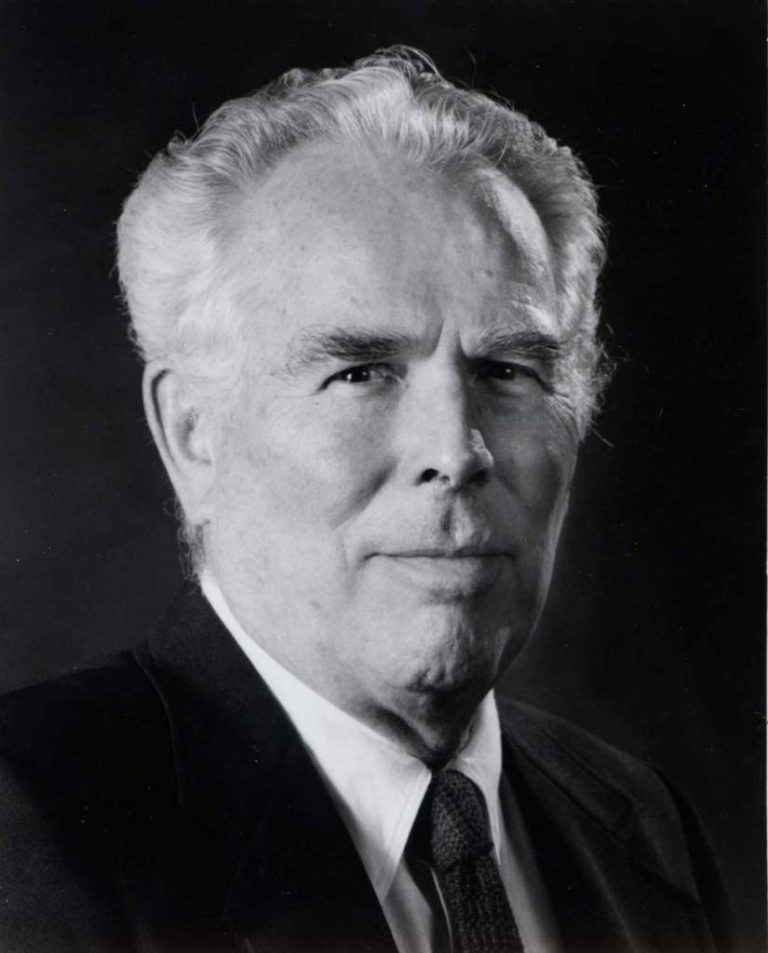
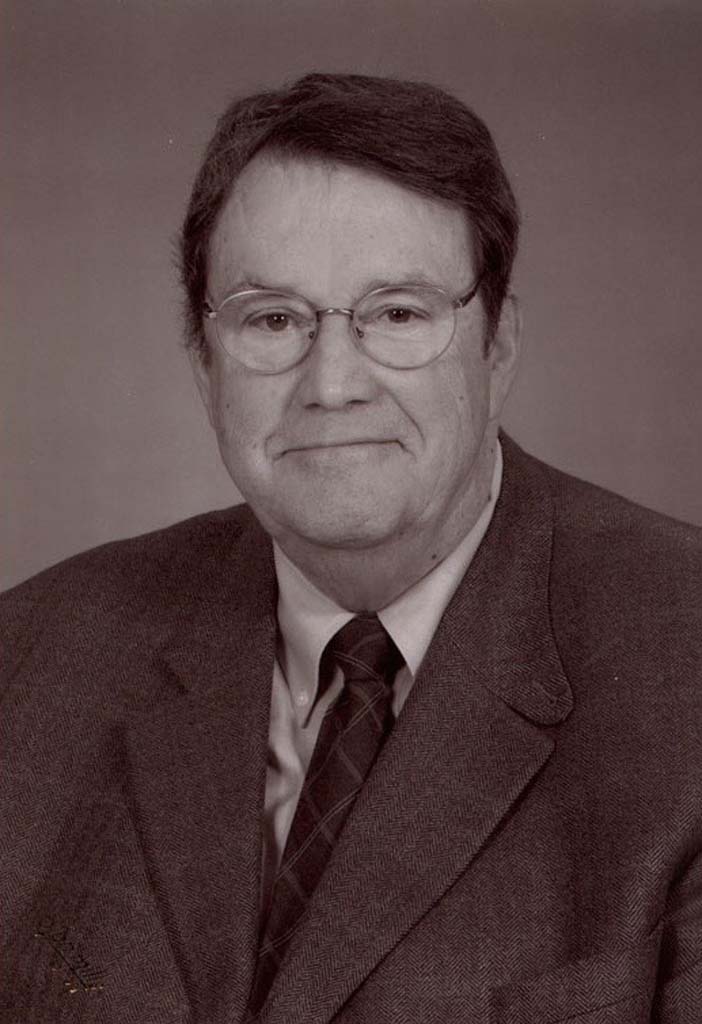
William F. Miller, MD, FAARC
William F. Miller, MD was very involved with the AARC and the profession. He was one of the giants in respiratory care who had profound impact on generations of respiratory therapists, nurses, physicians, and physical therapists. As a physician in Dallas, he was at the forefront of the respiratory therapy profession in this country, forming one of the first schools of respiratory therapy with 3 students in 1963. His vision for higher education of RTs was typical of his foresight. He was a founding member of the American Respiratory Care Foundation (ARCF) and his contributions there were innumerable. The Foundation and all it does today are a result of his leadership.
He was a recipient of the Jimmy A. Young Medal in 1979 and was also received honorary membership in the AARC. He served as a trustee for the ARCF for many years into the early 2000s. The William F. Miller Post-Graduate Education Recognition Award is named in his honor and established through his endowment.
He was a recipient of the Jimmy A. Young Medal in 1979 and was also received honorary membership in the AARC. He served as a trustee for the ARCF for many years into the early 2000s. The William F. Miller Post-Graduate Education Recognition Award is named in his honor and established through his endowment.


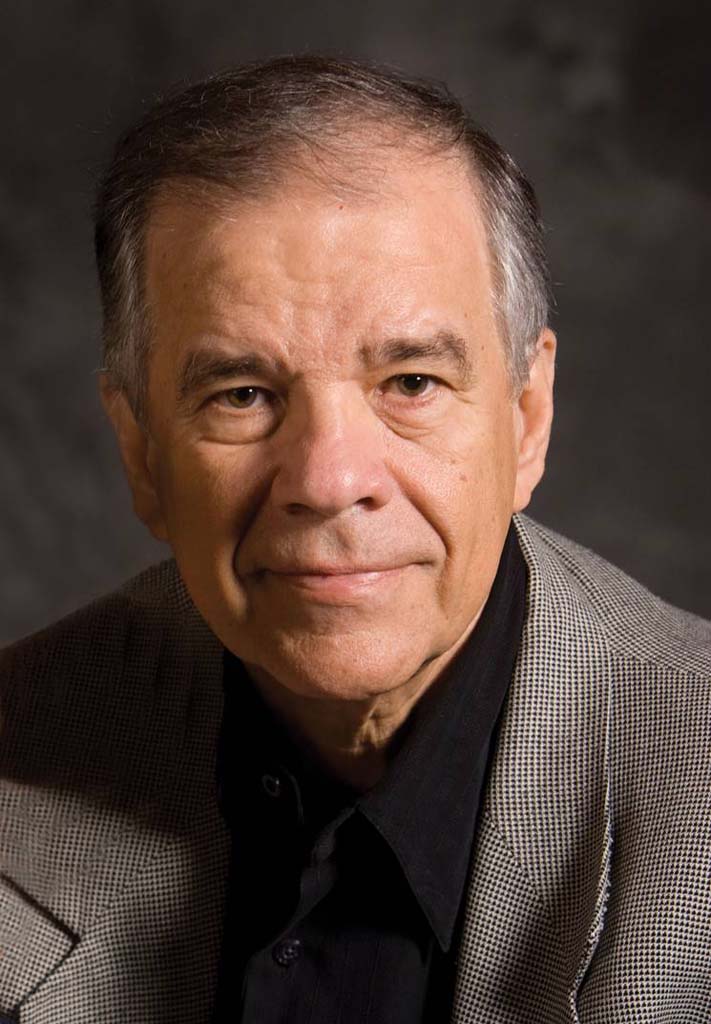
David J. Pierson, MD, FAARC
Dr. David Pierson is a gifted clinician, a superb teacher, a prolific author and mentor in respiratory care. He received his undergraduate degree from Oregon State University in 1965 with Bachelor’s degrees in Humanities and General Science. He then went on to medical school at John’s Hopkins University, graduating in 1969. He followed with an Internship and Residency in Internal Medicine at John’s Hopkins in 1971. He then did a Residency in Internal Medicine at the University of Colorado, 1972, and finished with a Fellowship in Pulmonary Medicine at the University of Colorado Medical Center in 1974 under Dr. Tom Petty. He is board certified in both Internal Medicine and Pulmonary Medicine.
His research interests have been in complications of mechanical ventilation and ICU care, particularly their clinical epidemiology and risk factors; respiratory care techniques, particularly clinical efficacy, cost-effectiveness, CQI, and educational issues; and writing, editing, and publishing in clinical medicine.
Dr. Pierson has been either the principal author or contributor to 118 publications. He has been a huge supporter of the field of Respiratory Therapy over the years. He was Medical Director for the Respiratory Care Department at Harborview Medical Center for over 30 years. He mentored the Respiratory Therapists there to utilize protocols, publish research, and utilize evidence-based medicine.
He became the editor for Respiratory Care Journal in 1998 and continued in that role for 10 years. His was committed to guiding the profession to embrace the research and evidence based medicine that has given the Respiratory Care Journal the recognition to be included in Pubmed. He continues as Editor Emeritus for the Respiratory Care Journal.
Dr. Pierson has advised and served on numerous AARC committees. Dr. Pierson was awarded honorary membership in the AARC and received the fellow designation (FAARC). He received the Jimmy A Young Medal in 2005.
The David J. Pierson, MD Award for Excellence in Education and Mentoring is named in his honor at the University of Washington. Dr. Pierson retired from the Division of Pulmonary and Critical Care Medicine at the University of Washington in 2011 and is currently an Emeritus Professor of Medicine.
His research interests have been in complications of mechanical ventilation and ICU care, particularly their clinical epidemiology and risk factors; respiratory care techniques, particularly clinical efficacy, cost-effectiveness, CQI, and educational issues; and writing, editing, and publishing in clinical medicine.
Dr. Pierson has been either the principal author or contributor to 118 publications. He has been a huge supporter of the field of Respiratory Therapy over the years. He was Medical Director for the Respiratory Care Department at Harborview Medical Center for over 30 years. He mentored the Respiratory Therapists there to utilize protocols, publish research, and utilize evidence-based medicine.
He became the editor for Respiratory Care Journal in 1998 and continued in that role for 10 years. His was committed to guiding the profession to embrace the research and evidence based medicine that has given the Respiratory Care Journal the recognition to be included in Pubmed. He continues as Editor Emeritus for the Respiratory Care Journal.
Dr. Pierson has advised and served on numerous AARC committees. Dr. Pierson was awarded honorary membership in the AARC and received the fellow designation (FAARC). He received the Jimmy A Young Medal in 2005.
The David J. Pierson, MD Award for Excellence in Education and Mentoring is named in his honor at the University of Washington. Dr. Pierson retired from the Division of Pulmonary and Critical Care Medicine at the University of Washington in 2011 and is currently an Emeritus Professor of Medicine.
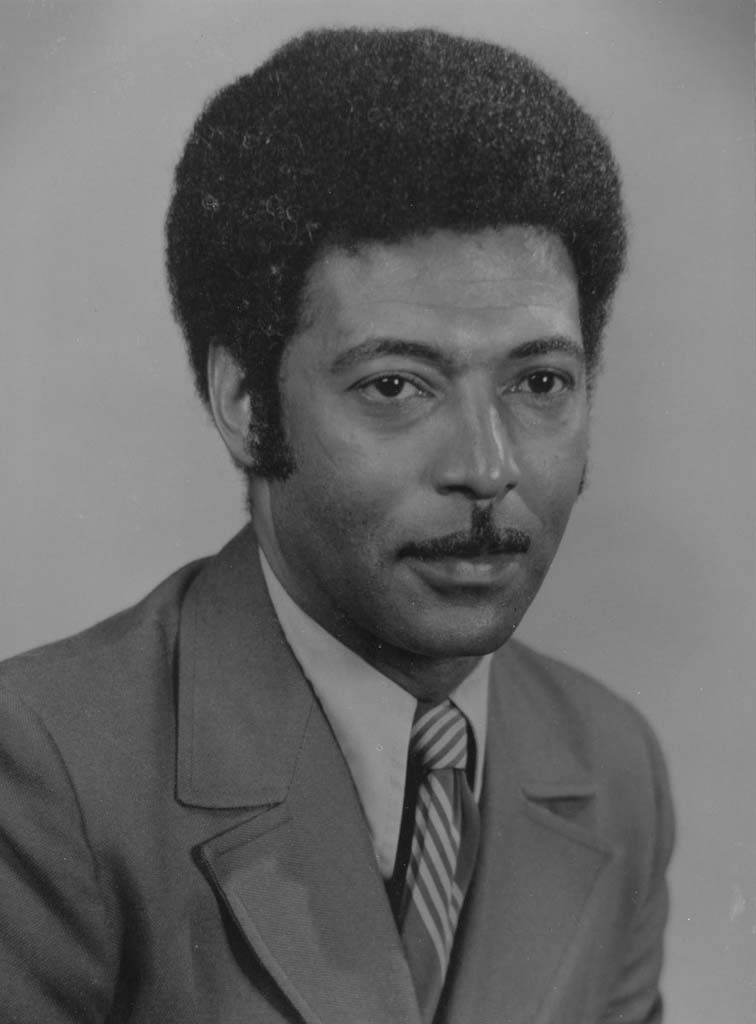

Jimmy A. Young, RRT
Jimmy Albert Young, MS, RRT was one of the profession’s most outstanding and dedicated leaders.
Jimmy Young served as Chief Inhalation Therapist at the Peter Bent Brigham Hospital in Boston. He earned the ARIT (registered Inhalation therapist) credential in 1965 and was assigned #263. He served in several roles including director of the education program at Northeastern University in Boston and became director of the Respiratory Therapy Department at Massachusetts General Hospital in 1970.
Along with Dean Crocker, Jimmy Young co-authored Principles and Practices of Inhalation Therapy, a textbook that was published in 1970.
He was elected to the Association's Board of Directors in 1968. He served the 22nd President of the American Association of Respiratory Therapy in 1973.
In 1975, he was serving as an NBRC Board of Trustee and member of the Executive Committee when he passed away unexpectedly.
The AARC presents the Jimmy A. Young Medal, the Association's highest honor, during the AARC International Congress.
Jimmy Young served as Chief Inhalation Therapist at the Peter Bent Brigham Hospital in Boston. He earned the ARIT (registered Inhalation therapist) credential in 1965 and was assigned #263. He served in several roles including director of the education program at Northeastern University in Boston and became director of the Respiratory Therapy Department at Massachusetts General Hospital in 1970.
Along with Dean Crocker, Jimmy Young co-authored Principles and Practices of Inhalation Therapy, a textbook that was published in 1970.
He was elected to the Association's Board of Directors in 1968. He served the 22nd President of the American Association of Respiratory Therapy in 1973.
In 1975, he was serving as an NBRC Board of Trustee and member of the Executive Committee when he passed away unexpectedly.
The AARC presents the Jimmy A. Young Medal, the Association's highest honor, during the AARC International Congress.


2016 Legends of Respiratory Care
Five new Legends were selected for the Class of 2016.


Vijay Deshpande, MS, RRT, FAARC
Vijay Deshpande has been an educator, author, and international lecturer for over four decades. He received numerous awards for his contributions at Georgia State University, from the Georgia Society for Respiratory Care, and the AARC.
Vijay was recognized as an AARC Fellow in 2000 and was awarded AARC Life Membership in 2009. He has been active on the AARC International Committee since 1990. He has lectured in over 20 countries. and has been instrumental in expanding respiratory care education in India. He has coauthored several textbooks on mechanical ventilation and contributed chapters to several others.
Vijay was recognized as an AARC Fellow in 2000 and was awarded AARC Life Membership in 2009. He has been active on the AARC International Committee since 1990. He has lectured in over 20 countries. and has been instrumental in expanding respiratory care education in India. He has coauthored several textbooks on mechanical ventilation and contributed chapters to several others.
Image provided by ViJay Deshpande

Ray Masferrer, RRT, FAARC
Ray Masferrer retired following 30-plus years as an Associate Executive Director of the AARC. However, he continues to serve as Managing Editor of the journal RESPIRATORY CARE, a position he first assumed in 1982 when he became a full-time employee of the AARC.
Prior to assuming his position with AARC, Ray served as a volunteer to the association, most notably chairing the then Publications Committee from 1971 to 1982, which at that time had oversight for the journal. One of Ray’s initial actions, in 1973 and in consort with the journal’s newly hired Editor-in-Chief Phil Kittredge, was to establish the first-ever Editorial Board. Mindful of Phil’s commitment to scientific inquiry and scholarly dissemination of research findings, Ray began a behind the scenes search to identify established researchers and authors to populate the Editorial Board. Such foresight elevated the stature of the journal and by association, positioned the profession as a logical companion, and in some cases, an alternative to, heretofore physician-only journals such as CHEST and THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE. Were it not for the cross-pollination resulting from Ray’s efforts, it is doubtful that the profession would enjoy today the enthusiastic support and active involvement of internationally recognized physicians.
Another major contribution of Ray was to establish the Journal Conferences, a legacy that stands today in which acknowledged experts are convened to focus on a specific topics of clinical relevance, with the resultant manuscripts published in RESPIRATORY CARE.
Aside from his lasting legacy as a primary contributor of the development of our journal, Ray was also responsible for the launch of several other important initiatives that further advanced the profession. In 1978, he worked with then AARC President Gary Gerard to form the Specialty Sections, and years later coordinated efforts to convert AARC’s clinical practice guidelines from expert opinion to evidence based.
Lastly, under Ray’s thoughtful and deliberate direction for three decades as AARC Director of Conventions, the AARC’s Annual Congress is now the world’s largest educational event for respiratory therapists. Furthermore, the annual Summer Forum has become a “go-to” event where managers and educators meet to develop strategies and tactics to address relevant issues and challenges to the profession.
Prior to assuming his position with AARC, Ray served as a volunteer to the association, most notably chairing the then Publications Committee from 1971 to 1982, which at that time had oversight for the journal. One of Ray’s initial actions, in 1973 and in consort with the journal’s newly hired Editor-in-Chief Phil Kittredge, was to establish the first-ever Editorial Board. Mindful of Phil’s commitment to scientific inquiry and scholarly dissemination of research findings, Ray began a behind the scenes search to identify established researchers and authors to populate the Editorial Board. Such foresight elevated the stature of the journal and by association, positioned the profession as a logical companion, and in some cases, an alternative to, heretofore physician-only journals such as CHEST and THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE. Were it not for the cross-pollination resulting from Ray’s efforts, it is doubtful that the profession would enjoy today the enthusiastic support and active involvement of internationally recognized physicians.
Another major contribution of Ray was to establish the Journal Conferences, a legacy that stands today in which acknowledged experts are convened to focus on a specific topics of clinical relevance, with the resultant manuscripts published in RESPIRATORY CARE.
Aside from his lasting legacy as a primary contributor of the development of our journal, Ray was also responsible for the launch of several other important initiatives that further advanced the profession. In 1978, he worked with then AARC President Gary Gerard to form the Specialty Sections, and years later coordinated efforts to convert AARC’s clinical practice guidelines from expert opinion to evidence based.
Lastly, under Ray’s thoughtful and deliberate direction for three decades as AARC Director of Conventions, the AARC’s Annual Congress is now the world’s largest educational event for respiratory therapists. Furthermore, the annual Summer Forum has become a “go-to” event where managers and educators meet to develop strategies and tactics to address relevant issues and challenges to the profession.


Theodore Oslick, MD, FAARC
Theodore Oslick, MD, FCCP, FAARC served on the NBRC Board of Trustees for 38 years, including 4 years as President.
In addition, Dr. Oslick served as Chair of over 20 committees for the NBRC and served as a member of over 35 NBRC committees.
Dr. Oslick has been designated Emeritus Trustee of the NBRC in recognition for his years of service and commitment to respiratory care credentialing.
Dr. Oslick was designated a Fellow (FAARC) of the AARC in 2007.
He is a past recipient of the NBRC's Albert H. Andrews Award and the NRBC's Sister Yvonne Jenn Award.
In addition, Dr. Oslick served as Chair of over 20 committees for the NBRC and served as a member of over 35 NBRC committees.
Dr. Oslick has been designated Emeritus Trustee of the NBRC in recognition for his years of service and commitment to respiratory care credentialing.
Dr. Oslick was designated a Fellow (FAARC) of the AARC in 2007.
He is a past recipient of the NBRC's Albert H. Andrews Award and the NRBC's Sister Yvonne Jenn Award.
Image provided by NBRC


Gregg Ruppel, MEd, RRT, FAARC
Gregg Ruppel, MEd, RRT, RPFT, FAARC is well-known for his contributions to pulmonary diagnostics over the past four decades.
Mr. Ruppel served on the NBRC Board of Trustees for 24 years, including 4 years as President. During his service on the NBRC Board, he chaired 12 committees and served on 18 other committees.
He authored nine editions of "Ruppel's Manual of Pulmonary Function Testing" as well as numerous articles in the Respiratory Care jorunal.
Gregg was inducted in the first class of AARC Fellows (FAARC) in 1998. He is also the recipient of the NBRC's Robert H. Miller Award and the NBRC's Sister Yvonne Jenn Award.
Mr. Ruppel served on the NBRC Board of Trustees for 24 years, including 4 years as President. During his service on the NBRC Board, he chaired 12 committees and served on 18 other committees.
He authored nine editions of "Ruppel's Manual of Pulmonary Function Testing" as well as numerous articles in the Respiratory Care jorunal.
Gregg was inducted in the first class of AARC Fellows (FAARC) in 1998. He is also the recipient of the NBRC's Robert H. Miller Award and the NBRC's Sister Yvonne Jenn Award.
Image provided by Gregg Ruppel


James Whitacre, MS, RRT
James Whitacre grew up in Ohio and graduated (in absentia) from Hiram College in pre-med with a minor in education. WWII interrupted his final year as he served as an Army corpsman in England, and Europe until 1945. He then returned to complete a Master of Science Degree from the University of Rochester; his thesis related to acetylcholine and the neuromuscular junction. Jim worked as a physiology lab instructor in the University’s Medical School.
In 1954 he transitioned to become director of the Hospital’s fledgling Inhalation Therapy Department. Fortunately the administration honored Jim’s frequent requests to attend national meetings. Besides learning more about clinical aspects of the profession, he began to volunteer to serve on various boards and committees. In 1955, he joined the American Association for Inhalation Therapy ( now AARC) and served its Board of Directors from 1956-60. Jim’s insights allowed him to see the importance of elevating the new professions’ standing through more rigorous educational standards, a formal credentialing and/or licensure system and delivery of improved technical services. He had the skills and energy to act on those insights.
In 1960 Jim was on the ground floor during formation of the American Registry for inhalation Therapy (now the NBRC) and become its first secretary. He was one of the first twelve people to pass the pilot exam administered in November of 1960. But because his name started with “W” and the ARIT’s incorporation was delayed until April of 1961, his registry number was 28. [Jim’s own signature was on his RRT certificate; students thought that was very “cool.”
In 1964 he moved to Pennsylvania to become Technical Director of the School of Inhalation Therapists at the Health Center Hospitals in Pittsburgh and instructor with the University of Pittsburgh. The “father of CPR and ICU medicine,” Dr. Peter Safar was his medical director.
Jim served as the first editor of the AAIT's journal, Inhalation Therapy which began in 1956. He continued to serve as journal editor until 1967. Jim was also involved in writing textbooks and was a chapter contributor and editor the textbook Respiratory Therapy by Dr. Peter Safar’s.
Jim’s career as an educator in respiratory care began in Rochester and evolved further in Pittsburg. A big change came in 1967 when he moved to Columbia, Missouri to establish the first baccalaureate degree program west of the Mississippi. Jim served as the "Mizzou" program director and teacher until 1980.
The work Jim did with the credentialing system likely provided some background for the contributions he made to the educational accreditation system. He served on the Joint Review Committee for Inhalation Therapy Education (JRCRTE) from 1969-1971.
In 1954 he transitioned to become director of the Hospital’s fledgling Inhalation Therapy Department. Fortunately the administration honored Jim’s frequent requests to attend national meetings. Besides learning more about clinical aspects of the profession, he began to volunteer to serve on various boards and committees. In 1955, he joined the American Association for Inhalation Therapy ( now AARC) and served its Board of Directors from 1956-60. Jim’s insights allowed him to see the importance of elevating the new professions’ standing through more rigorous educational standards, a formal credentialing and/or licensure system and delivery of improved technical services. He had the skills and energy to act on those insights.
In 1960 Jim was on the ground floor during formation of the American Registry for inhalation Therapy (now the NBRC) and become its first secretary. He was one of the first twelve people to pass the pilot exam administered in November of 1960. But because his name started with “W” and the ARIT’s incorporation was delayed until April of 1961, his registry number was 28. [Jim’s own signature was on his RRT certificate; students thought that was very “cool.”
In 1964 he moved to Pennsylvania to become Technical Director of the School of Inhalation Therapists at the Health Center Hospitals in Pittsburgh and instructor with the University of Pittsburgh. The “father of CPR and ICU medicine,” Dr. Peter Safar was his medical director.
Jim served as the first editor of the AAIT's journal, Inhalation Therapy which began in 1956. He continued to serve as journal editor until 1967. Jim was also involved in writing textbooks and was a chapter contributor and editor the textbook Respiratory Therapy by Dr. Peter Safar’s.
Jim’s career as an educator in respiratory care began in Rochester and evolved further in Pittsburg. A big change came in 1967 when he moved to Columbia, Missouri to establish the first baccalaureate degree program west of the Mississippi. Jim served as the "Mizzou" program director and teacher until 1980.
The work Jim did with the credentialing system likely provided some background for the contributions he made to the educational accreditation system. He served on the Joint Review Committee for Inhalation Therapy Education (JRCRTE) from 1969-1971.
A special thanks to Jeff Ward for supplying the biographical information for James Whitacre.


2017 Legends of Respiratory Care
Four Legends were named in the Class of 2017.


Mary Ellen Avery, MD
Dr. Avery (1927-2011) held numerous roles during her career including researcher, clinician, educator, and administrator.
Dr. Avery became especially interested in pulmonary medicine following her diagnosis with tuberculosis shortly after she graduated from medical school in 1952.
In the late 1950s, Dr. Avery was a pioneer in research that helped lead to the discovery of surfactant deficiency in respiratory distress syndrome (RDS) in premature babies and led research in surfactant replacement therapy.
Dr. Avery had a strong interest in helping train young physicians, particularly in pulmonary disease and neonatology. She was the first woman to chair a clinical department at Harvard Medical School.
In 1990–91, Dr. Avery was the President of the American Pediatric Society. She was active in numerous national and international professional associations and organizations, including UNICEF.
Dr. Avery became especially interested in pulmonary medicine following her diagnosis with tuberculosis shortly after she graduated from medical school in 1952.
In the late 1950s, Dr. Avery was a pioneer in research that helped lead to the discovery of surfactant deficiency in respiratory distress syndrome (RDS) in premature babies and led research in surfactant replacement therapy.
Dr. Avery had a strong interest in helping train young physicians, particularly in pulmonary disease and neonatology. She was the first woman to chair a clinical department at Harvard Medical School.
In 1990–91, Dr. Avery was the President of the American Pediatric Society. She was active in numerous national and international professional associations and organizations, including UNICEF.
Bachrach Studios
Roger C. Bone, MD, MACP, MFCP, FCCM
Dr. Roger C. Bone was a lung specialist and former President of the Medical College of Ohio. He spent his final year reminding his fellow physicians about their obligations toward the terminally ill. He wrote many medical journals and appeared on network television, asking his peers to show greater consideration for patients dying under their care.
As a lung specialist, Dr. Bone published some 1,000 scientific articles and wrote or edited 56 books. His “Pulmonary and Critical Care Medicine” went through several editions.
Dr. Bone was awarded AARC Honorary Membership.
As a lung specialist, Dr. Bone published some 1,000 scientific articles and wrote or edited 56 books. His “Pulmonary and Critical Care Medicine” went through several editions.
Dr. Bone was awarded AARC Honorary Membership.

Walter J. O'Donohue, Jr., MD
Dr. Walter J. O'Donohue, Jr. held key roles in numerous national organizations including the AARC, NAMDRC, NBRC, ALA, ACCP, ATS, and AMA. He served as President of NBRC. He was a charter member of BOMA. Dr. O'Donohue was awarded AARC Honorary membership. He authored/edited four textbooks, contributed 150 scientific journal articles, and delivered over 300 presentations at national and international conferences. Many of his publications focused on oxygen therapy and appeared in the RESPIRATORY CARE journal. Dr. O'Donohue was the physician member on the AARC's first Clinical Practice Guidelines Committee and participated in the development of the AARC's initial CPG entitled "Oxygen Therapy in the Acute Care Setting"


Margaret Traband, MEd, RRT, FAARC
A member of the AARC since 1972, Margaret "Peg" Traband served as AARC Treasurer, Secretary, and President as well as chairing the PAC. She also served on the NBRC BOD from 1990-1997 which included a term as President in (1994-1995). Peg worked with the NBRC on examination committees for Neo/Peds, advanced practice, entry level, and clinical simulation. She has been awarded many of respiratory care's most prestigious awards including:
•NBRC Robert Miller
•AARC Fellow
•AARC Life membership
•AARC Jimmy A Young Medal
Peg also has many respiratory publications to her name as well as numerous speaking engagements on respiratory therapy related topics and the issues that face the profession. She has countless hours of volunteerism not only to respiratory therapist and students but also to the patients we serve. Peg has been a mentor to new therapists and provides a calming voice to the patients.
•NBRC Robert Miller
•AARC Fellow
•AARC Life membership
•AARC Jimmy A Young Medal
Peg also has many respiratory publications to her name as well as numerous speaking engagements on respiratory therapy related topics and the issues that face the profession. She has countless hours of volunteerism not only to respiratory therapist and students but also to the patients we serve. Peg has been a mentor to new therapists and provides a calming voice to the patients.


Class of 2018 Legends
Five Legends were named for the Class of 2018.


Albert Aranson, MD
In virtually every state in the United States, there were legends of respiratory care who had an historic impact on the profession. Some of them were the first medical directors of Respiratory Therapy departments, who acted locally to initiate and develop the profession, but whose actions eventually were felt globally. Were it not for these medical directors, the profession of respiratory care might never have come to be. And so, it was with Dr. Albert Aranson, the first formally trained pulmonologist in the State of Maine, who was Maine's pioneer of both Respiratory Therapy and Pulmonary and Critical Care Medicine. In essence, he was the history of those fields in the State of Maine.
In 1947, immediately out of fellowship training at the Cushing VAMC in Framingham, MA, Dr. Aranson became its Chief of Pulmonary Medicine, an advancement unheard of in those days. Upon his arrival in 1949 at Maine Medical Center (MMC), the state’s largest hospital, Dr. Aranson founded Maine’s first Pulmonary Division, Pulmonary Function Laboratory, and Inhalation Therapy Department (as it was called in those days). He hired Maine’s first PFT tech, Virginia Charlton, and Maine’s first respiratory therapist, Robert H. Miller, RRT, the first RT to become president of the NBRC and for whom the NBRC award is named. Mr. Miller was director of MMC’s Respiratory Therapy Department for more than 25 years.
In the 1950s and 1960s, Dr. Aranson obtained grant money from the federal government and from the York and Cumberland County TB & Health Associations to fund projects at MMC for the study of obstructive lung diseases and the measurement of pulmonary function in health and disease, in which respiratory therapists were intimately involved. These grant monies funded expansion of the then Inhalation Therapy Department, training of respiratory therapists and pulmonary function technologists, establishment of a new Intensive Care Unit (ICU), and development of the state’s first TB Clinic, which he founded in 1949 and directed until his retirement. He also created the Respiratory Therapy Department, Pulmonary Function Laboratory, and Maine’s first ICU at Portland's Mercy Hospital.
Dr. Aranson was one of the first physicians in the country to use streptomycin, the first drug used for the treatment of tuberculosis (TB). As Maine’s chief TB consultant, Dr. Aranson helped develop protocols for the modern antibiotic treatment of TB, as well as TB control and prevention protocols for the State of Maine Department of Health, involving RTs in the process. He served as TB consultant during his entire medical career in Maine.
Dr. Aranson had a long and prolific alliance with the American Lung Association of Maine, including involvement in anti-smoking campaigns and TB prevention and control, in which RTs participated. In the 1960s, Dr. Aranson was responsible for the removal of cigarette vending machines at MMC, a movement far ahead of his time that spread throughout the state.
As Director of Medical Education at MMC, Dr. Aranson trained hundreds of students of respiratory therapy, nursing, and medicine, as well as residents and pulmonary fellows, many of whom, because of his encouragement, chose to settle in Maine, including in underserved areas, to care for the state’s citizens. In the training of these students, Dr. Aranson inculcated care for the patient first and foremost, a legendary philosophy for which he is remembered by all who came under his tutelage.
In summary, Dr. Albert Aranson was truly a legend as Maine’s pioneer of Respiratory Therapy and Pulmonary and Critical Care Medicine, just one piece of meaningful, consequential, and historical impact on respiratory care nationwide.
In 1947, immediately out of fellowship training at the Cushing VAMC in Framingham, MA, Dr. Aranson became its Chief of Pulmonary Medicine, an advancement unheard of in those days. Upon his arrival in 1949 at Maine Medical Center (MMC), the state’s largest hospital, Dr. Aranson founded Maine’s first Pulmonary Division, Pulmonary Function Laboratory, and Inhalation Therapy Department (as it was called in those days). He hired Maine’s first PFT tech, Virginia Charlton, and Maine’s first respiratory therapist, Robert H. Miller, RRT, the first RT to become president of the NBRC and for whom the NBRC award is named. Mr. Miller was director of MMC’s Respiratory Therapy Department for more than 25 years.
In the 1950s and 1960s, Dr. Aranson obtained grant money from the federal government and from the York and Cumberland County TB & Health Associations to fund projects at MMC for the study of obstructive lung diseases and the measurement of pulmonary function in health and disease, in which respiratory therapists were intimately involved. These grant monies funded expansion of the then Inhalation Therapy Department, training of respiratory therapists and pulmonary function technologists, establishment of a new Intensive Care Unit (ICU), and development of the state’s first TB Clinic, which he founded in 1949 and directed until his retirement. He also created the Respiratory Therapy Department, Pulmonary Function Laboratory, and Maine’s first ICU at Portland's Mercy Hospital.
Dr. Aranson was one of the first physicians in the country to use streptomycin, the first drug used for the treatment of tuberculosis (TB). As Maine’s chief TB consultant, Dr. Aranson helped develop protocols for the modern antibiotic treatment of TB, as well as TB control and prevention protocols for the State of Maine Department of Health, involving RTs in the process. He served as TB consultant during his entire medical career in Maine.
Dr. Aranson had a long and prolific alliance with the American Lung Association of Maine, including involvement in anti-smoking campaigns and TB prevention and control, in which RTs participated. In the 1960s, Dr. Aranson was responsible for the removal of cigarette vending machines at MMC, a movement far ahead of his time that spread throughout the state.
As Director of Medical Education at MMC, Dr. Aranson trained hundreds of students of respiratory therapy, nursing, and medicine, as well as residents and pulmonary fellows, many of whom, because of his encouragement, chose to settle in Maine, including in underserved areas, to care for the state’s citizens. In the training of these students, Dr. Aranson inculcated care for the patient first and foremost, a legendary philosophy for which he is remembered by all who came under his tutelage.
In summary, Dr. Albert Aranson was truly a legend as Maine’s pioneer of Respiratory Therapy and Pulmonary and Critical Care Medicine, just one piece of meaningful, consequential, and historical impact on respiratory care nationwide.


Dean Hess, PhD, RRT, FAARC
Dr. Dean Hess’ area of clinical expertise and innovation is in adult mechanical ventilation. Supporting activities include editorial boards and books, investigation, and professional society activities. He has been invited to lecture on mechanical ventilation at many major international meetings including the American Thoracic Society, the Society for Critical Care Medicine, the American Association for Respiratory Care, the American College of Chest Physicians, the American College of Physicians, the Society of Thoracic Surgery, the International Society for Aerosols in Medicine, the European Respiratory Society, and others. He has been a visiting professor at academic institutions in the United States and Southeast Asia. Dr. Hess does 3 hours of lectures on mechanical ventilation for the residents in the Medical ICU every month, and provide lectures on a regular basis to critical care fellows in the various training MGH programs.
Dr. Hess is Editor in Chief of RESPIRATORY CARE, the peer-reviewed international journal of the American Association for Respiratory Care. He is also a member of the Editorial Boards for the Journal of Aerosol Medicine and Pulmonary Drug Delivery and Simulation in Healthcare. Dr. Hess is the first author of “Essentials of Mechanical Ventilation” (3rd edition in preparation) and “Respiratory Care Principles and Practice” (3rd edition). He has had leadership roles and served on committees in national and international professional organizations. He is also part of the management team of the Respiratory Care Department at the Massachusetts General Hospital, which is arguably the best respiratory care department in the country, with a staff of about 100 persons. For more than 10 years, he has had a sustained national and international reputation as a leader and innovator in the field of mechanical ventilation specifically, and in the wider field of respiratory care. This has had significant influence on practice as a result of his teaching, scholarship and innovation.
Dr. Hess is Editor in Chief of RESPIRATORY CARE, the peer-reviewed international journal of the American Association for Respiratory Care. He is also a member of the Editorial Boards for the Journal of Aerosol Medicine and Pulmonary Drug Delivery and Simulation in Healthcare. Dr. Hess is the first author of “Essentials of Mechanical Ventilation” (3rd edition in preparation) and “Respiratory Care Principles and Practice” (3rd edition). He has had leadership roles and served on committees in national and international professional organizations. He is also part of the management team of the Respiratory Care Department at the Massachusetts General Hospital, which is arguably the best respiratory care department in the country, with a staff of about 100 persons. For more than 10 years, he has had a sustained national and international reputation as a leader and innovator in the field of mechanical ventilation specifically, and in the wider field of respiratory care. This has had significant influence on practice as a result of his teaching, scholarship and innovation.


Alan H. Jobe, MD, PhD
Dr. Alan H. Jobe is currently the Professor of Pediatrics, University of Cincinnati, Children’s Hospital Medical Center, Cincinnati, OH. Dr. Jobe performed many of the metabolic and physiologic studies that resulted in FDA approval of surfactant for the treatment of Respiratory Distress Syndrome. His research interests are in surfactant homeostasis, lung injury and Bronchopulmonary Dysplasia, fetal inflammation, and lung development. He was the Chair of the Pediatric Assembly of the American Thoracic Society in 1986 and was Chair of the ATS Research Fellowship Review Committee from 1992-1995. Other activities include reviewing grants for the Basil O’Conner Awards for March of Dimes. He became a member of The American Society for Clinical Investigation in 1986.
Dr. Jobe received the Ross Award in Research from the Western Society for Pediatric Research in 1984 and the E Mead Johnson Award for Pediatric Research in 1986. He received the Arvo Ylppö Medal for Pediatric Research from the Finnish Pediatric Societies in Helsinki in 2002. He was voted the George Simbruner Lecturing Award at New Frontiers in Neonatology in Innsbruck, Austria in 2005. Dr. Jobe was elected to the Institute of Medicine (National Academy of Medicine) in 2007. He gave the William Silverman Lectureship at the PAS meeting in 2009. He received the Thomas Hazinski Distinguished Service Award from the Society for Pediatric Research in 2010. In 2011, he was recognized by LA BioMed at Harbor-UCLA Medical Center as a Legend for service to Harbor-UCLA. He received the Virginia Apgar Award from the AAP for 2011. He also was recognized by the Founders Award from the Midwestern Society for Pediatric Research in 2012. In 2017 he received the Mary Ellen Avery Neonatal Research Award from the SPR and the APS.
Dr. Jobe received the Ross Award in Research from the Western Society for Pediatric Research in 1984 and the E Mead Johnson Award for Pediatric Research in 1986. He received the Arvo Ylppö Medal for Pediatric Research from the Finnish Pediatric Societies in Helsinki in 2002. He was voted the George Simbruner Lecturing Award at New Frontiers in Neonatology in Innsbruck, Austria in 2005. Dr. Jobe was elected to the Institute of Medicine (National Academy of Medicine) in 2007. He gave the William Silverman Lectureship at the PAS meeting in 2009. He received the Thomas Hazinski Distinguished Service Award from the Society for Pediatric Research in 2010. In 2011, he was recognized by LA BioMed at Harbor-UCLA Medical Center as a Legend for service to Harbor-UCLA. He received the Virginia Apgar Award from the AAP for 2011. He also was recognized by the Founders Award from the Midwestern Society for Pediatric Research in 2012. In 2017 he received the Mary Ellen Avery Neonatal Research Award from the SPR and the APS.


Edwin R. Levine, MD, FCCP
Edwin R. Levine, M.D. is credited with establishing the first on-the-job training program for inhalation therapy. It was established at the Michael Reese Hospital in Chicago Illinois in 1943. Dr. Levine and his colleagues provided didactic and clinical instruction for the program and was one of the founders of the Inhalation Therapy Association, the predecessor of the American Association for Respiratory Care. He authored numerous journal articles and presented at numerous scientific conferences. He served as the Medical Director at Edgewater Hospital, Chicago, IL which was among the first accredited inhalation therapy training programs in the US.
In 1952, Dr. Levine held the position of President of the Inhalation Therapy Association (ITA). In our 70+ years of existence, Dr. Levine is the only physician to be President of our Association.
In 1952, Dr. Levine held the position of President of the Inhalation Therapy Association (ITA). In our 70+ years of existence, Dr. Levine is the only physician to be President of our Association.
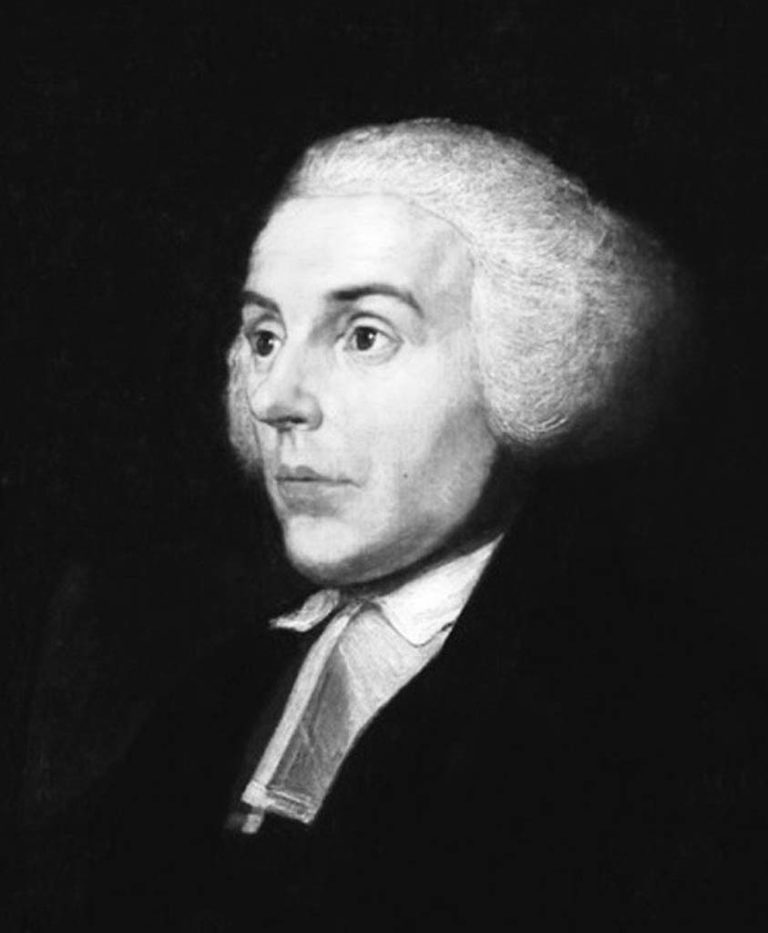

Joseph Priestley, LLD, FRS
Joseph Priestley (1733–1804) was an English clergyman, political theorist and physical scientist. His work contributed to advances in political and religious thought. He is best known for his contribution to the chemistry of gases and has been credited with the discovery of oxygen after having isolated it in a gaseous state. He also invented soda water, wrote about electricity.
In the 1770s, Priestley began his research into the nature and properties of gases. He began examining all the “airs” that might be released from different substances. In his pursuits, Priestley identified eight gases and this record has never been equaled before or after his discoveries. Priestley’s most important gas discovery was what he called “dephlogisticated air” or oxygen as we know it. The name “oxygen” would be coined later by Antoine-Laurent Lavoisier. His work appears to have been the predecessor to what the world would come to know as photosynthesis and respiration.
Some timeline history of Joseph Priestley:
March 13, 1733 - Born in Birstall Fieldhead, near Leeds, Yorkshire, England.
1752 – Entered the Dissenting Academy at Daventry, Northamptonshire to be educated in philosophy, science, languages and literature. It is here where he became a radical freethinker in religion.
1755-1761 – Ministered at Needham Market, Suffolk and at Nantwich, Cheshire.
1762 – Ordained a Dissenting minister. Married to Mary Wilkinson (they had one daughter and three sons).
1765 – Met Benjamin Franklin and Priestley’s interest in science intensifies.
1767 – “History of Electricity” was his first scientific work.
1770s – Began his work on the nature and properties of gases.
1791 - His openly expressed views as a minister were considered seditious by both the English authorities and citizens. They destroyed his house and laboratory. This event was the deciding factor that led him to emigrate to the United States.
1794 – Arrived in the United States
February 6, 1804 - Died in Northumberland, PA, U.S.
In the 1770s, Priestley began his research into the nature and properties of gases. He began examining all the “airs” that might be released from different substances. In his pursuits, Priestley identified eight gases and this record has never been equaled before or after his discoveries. Priestley’s most important gas discovery was what he called “dephlogisticated air” or oxygen as we know it. The name “oxygen” would be coined later by Antoine-Laurent Lavoisier. His work appears to have been the predecessor to what the world would come to know as photosynthesis and respiration.
Some timeline history of Joseph Priestley:
March 13, 1733 - Born in Birstall Fieldhead, near Leeds, Yorkshire, England.
1752 – Entered the Dissenting Academy at Daventry, Northamptonshire to be educated in philosophy, science, languages and literature. It is here where he became a radical freethinker in religion.
1755-1761 – Ministered at Needham Market, Suffolk and at Nantwich, Cheshire.
1762 – Ordained a Dissenting minister. Married to Mary Wilkinson (they had one daughter and three sons).
1765 – Met Benjamin Franklin and Priestley’s interest in science intensifies.
1767 – “History of Electricity” was his first scientific work.
1770s – Began his work on the nature and properties of gases.
1791 - His openly expressed views as a minister were considered seditious by both the English authorities and citizens. They destroyed his house and laboratory. This event was the deciding factor that led him to emigrate to the United States.
1794 – Arrived in the United States
February 6, 1804 - Died in Northumberland, PA, U.S.
Image from Dennis Glover


Class of 2019 Legends
Five new Legends were named for the Class of 2019.
Leland Clark, PhD
Leland Clark, PhD was an American biochemist born in Rochester, New York. He is most well known as the inventor of the Clark electrode, a device used for measuring oxygen in blood, water and other liquids. Clark is considered the "father of biosensors", and the modern-day glucose sensor used daily by millions of diabetics is based on his research. He conducted pioneering research on heart-lung machines in the 1940s and '50s and was holder of more than 25 patents. Although he developed a fluorocarbon-based liquid that could be breathed successfully by mice in place of air, his lifelong goal of developing artificial blood remained unfulfilled at the time of his death. He is the inventor of Oxycyte, a third-generation perfluorocarbon (PFC) therapeutic oxygen carrier designed to enhance oxygen delivery to damaged cells.
Clark received his B.S. degree in Chemistry from Antioch College in 1941 and his Ph.D. in Biochemistry and Physiology from the University of Rochester in 1944. Clark began his professional career as an Assistant Professor of biochemistry at his alma mater, Antioch College, in Yellow Springs, Ohio. When he left Antioch in 1958, he was head of the department. From 1955 to 1958, he held a simultaneous appointment the University of Cincinnati College of Medicine as a Senior In 1958, Clark moved to the University of Alabama Medical College as an associate professor of biochemistry. He later became professor of biochemistry in the same department. Clark became professor of research pediatrics at the Cincinnati Children’s Hospital Research Foundation in 1968 and remained there until he retired in 1991. Afterwards, he helped to found the company Synthetic Blood International, now known as Oxygen Biotherapeutics, Inc., which markets his invention Oxycyte. Other Clark inventions were put into production and marketed by Yellow Springs Instrument Company. He was a founding member of the Editorial Board of the scientific journal Biosensors & Bioelectronics in 1985.
Dr. Clark received the following recognition for his work: National Research Council Fellowship (1941). NIH Research Career Award (1962). Distinguished Lecturer Award, American College of Chest Physicians (1975). Honorary Doctor of Science, University of Rochester School of Medicine and Dentistry (1984). Horace Mann Award for Service to Humanity, Antioch College (1984). Heyrovsky Award in Recognition of the Invention of the Membrane-Covered Polarographic Oxygen Electrode (1985). American Association for Clinical Chemistry Award for Outstanding Contributions to Clinical Chemistry (1989). American Heart Association Samuel Kaplan Visionary Award (1991). Enshrinement into the Engineering and Science Hall of Fame (1991). Pharmacia Biosensor’s Sensational Contributions to the Advancement of Biosensor Technology Award (1992). Daniel Drake Award for Outstanding Achievements in Research, University of Cincinnati College of Medicine (1993). Elected to the National Academy of Engineering (1995). National Academy of Engineering Fritz J. and Dolores H. Russ Prize (2005).
Clark received his B.S. degree in Chemistry from Antioch College in 1941 and his Ph.D. in Biochemistry and Physiology from the University of Rochester in 1944. Clark began his professional career as an Assistant Professor of biochemistry at his alma mater, Antioch College, in Yellow Springs, Ohio. When he left Antioch in 1958, he was head of the department. From 1955 to 1958, he held a simultaneous appointment the University of Cincinnati College of Medicine as a Senior In 1958, Clark moved to the University of Alabama Medical College as an associate professor of biochemistry. He later became professor of biochemistry in the same department. Clark became professor of research pediatrics at the Cincinnati Children’s Hospital Research Foundation in 1968 and remained there until he retired in 1991. Afterwards, he helped to found the company Synthetic Blood International, now known as Oxygen Biotherapeutics, Inc., which markets his invention Oxycyte. Other Clark inventions were put into production and marketed by Yellow Springs Instrument Company. He was a founding member of the Editorial Board of the scientific journal Biosensors & Bioelectronics in 1985.
Dr. Clark received the following recognition for his work: National Research Council Fellowship (1941). NIH Research Career Award (1962). Distinguished Lecturer Award, American College of Chest Physicians (1975). Honorary Doctor of Science, University of Rochester School of Medicine and Dentistry (1984). Horace Mann Award for Service to Humanity, Antioch College (1984). Heyrovsky Award in Recognition of the Invention of the Membrane-Covered Polarographic Oxygen Electrode (1985). American Association for Clinical Chemistry Award for Outstanding Contributions to Clinical Chemistry (1989). American Heart Association Samuel Kaplan Visionary Award (1991). Enshrinement into the Engineering and Science Hall of Fame (1991). Pharmacia Biosensor’s Sensational Contributions to the Advancement of Biosensor Technology Award (1992). Daniel Drake Award for Outstanding Achievements in Research, University of Cincinnati College of Medicine (1993). Elected to the National Academy of Engineering (1995). National Academy of Engineering Fritz J. and Dolores H. Russ Prize (2005).

Allen DeVilbiss, MD
Dr. Allen DeVilbiss was a nose and throat specialist who invented the first atomizer in the late 1880’s to provide an easier way to apply medicines to patients' throats. Dr. DeVilbiss tried harder, worked smarter and became an innovator – dedicated to the quality of design and its impact on the quality of life. He would tinker around in his backyard woodshed until just the right tool was perfected. His invention was so successful that by 1890 he had retired from medical practice and established a company, DeVilbiss Manufacturing Company, to produce the atomizers. This item carries patent dates from 1907 to 1916. The company produced many surgical instruments of the time.


John Hutchinson, MBBS
John Hutchinson invented the spirometer, a device for measuring lung capacity. He used this device in evaluating candidates for life insurance while working as a physician to the Brittania Life office. Today, the spirometer is the backbone of pulmonary function laboratories around the world.
He also theorized that air pollution could lead to poor health. Particularly, he researched the safety of coal mining and the presence of charcoal in miner's lungs. He moved to Australia around 1852, and then later to Fiji where he died as a result of contracting dysentery.
John Hutchinson, a surgeon, recognized that the volume of air that can be exhaled from fully inflated lungs is a powerful indicator of longevity. He invented the spirometer to measure what he called the vital capacity, ie, the capacity to live. Much later, the concept of the timed vital capacity, which became known as the FEV1, was added. Together, these two numbers, vital capacity and FEV1, are useful in identifying patients at risk of many diseases, including COPD, lung cancer, heart attack, stroke, and all-cause mortality.
He also theorized that air pollution could lead to poor health. Particularly, he researched the safety of coal mining and the presence of charcoal in miner's lungs. He moved to Australia around 1852, and then later to Fiji where he died as a result of contracting dysentery.
John Hutchinson, a surgeon, recognized that the volume of air that can be exhaled from fully inflated lungs is a powerful indicator of longevity. He invented the spirometer to measure what he called the vital capacity, ie, the capacity to live. Much later, the concept of the timed vital capacity, which became known as the FEV1, was added. Together, these two numbers, vital capacity and FEV1, are useful in identifying patients at risk of many diseases, including COPD, lung cancer, heart attack, stroke, and all-cause mortality.


B. Marie Krogh, MD
Birte Marie Krogh was born on 25 December 1874 in Vosegaard, Denmark, one of only four of nine children in her family to survive to adulthood. Due to family pressure, she was not able to attend a university-preparatory school until 1898, graduating three years later. While attending the University of Copenhagen, she met and married (1904) August Krogh, the future Nobel Laureate in physiology, in a physiology class. After Krogh graduated with her medical degree in 1907, the couple began their life-long collaboration with an expedition to Greenland to measure respiration and gas exchange in the meat-eating Inuit of the island.
Over the next two years, the couple used themselves as experimental subjects studying gas diffusion in the lungs. Marie took the novel step to use CO as a surrogate for O2 in many of these studies - the forerunner of the modern DLCO test.. The goal was to determine if the rate of O2 diffusion was sufficient to account for the O2 uptake even at high altitudes or during various pulmonary diseases. Thirty-five years later the CO uptake method, as described by Marie Krogh, was rediscovered and is now used extensively as a clinical test. Indeed, the rate constant for CO uptake is termed the Krogh constant (Kco).
Her husband, August, in his continued studies of respiration in animals and humans, became interested in the delivery of O2 from the capillaries to the tissue. The studies that followed led to his discovery of the regulation of capillary circulation, for which he was awarded the Nobel Prize in 1920.
Marie earned the advanced Dr. med. from the University of Copenhagen in 1914, only the fourth woman in Denmark to receive an advanced medical degree. Her youngest daughter, Bodil Schmidt-Nielsen, later became an eminent physiologist in her own right.
After she developed diabetes in the early 1920s, the couple began researching insulin production and developed a profitable technique that allowed them to start a pharmaceutical company that spent its profits on physiological and endocrinological research.
Over the next two years, the couple used themselves as experimental subjects studying gas diffusion in the lungs. Marie took the novel step to use CO as a surrogate for O2 in many of these studies - the forerunner of the modern DLCO test.. The goal was to determine if the rate of O2 diffusion was sufficient to account for the O2 uptake even at high altitudes or during various pulmonary diseases. Thirty-five years later the CO uptake method, as described by Marie Krogh, was rediscovered and is now used extensively as a clinical test. Indeed, the rate constant for CO uptake is termed the Krogh constant (Kco).
Her husband, August, in his continued studies of respiration in animals and humans, became interested in the delivery of O2 from the capillaries to the tissue. The studies that followed led to his discovery of the regulation of capillary circulation, for which he was awarded the Nobel Prize in 1920.
Marie earned the advanced Dr. med. from the University of Copenhagen in 1914, only the fourth woman in Denmark to receive an advanced medical degree. Her youngest daughter, Bodil Schmidt-Nielsen, later became an eminent physiologist in her own right.
After she developed diabetes in the early 1920s, the couple began researching insulin production and developed a profitable technique that allowed them to start a pharmaceutical company that spent its profits on physiological and endocrinological research.

John W. Severinghaus, MD
Dr. Severinghaus is Professor Emeritus of Anesthesia at the University of California in San Francisco. He was a Senior Staff Member of the Cardiovascular Research Institute. He was born in Madison, Wisconsin on May 6, 1922. After majoring in physics he designed radar test equipment at MIT during World War II During medical school he developed the first electrophrenic respirators. He published the first measurements of the rate of uptake of N2O during anesthesia.
From 1953-1958, he was chief of anesthesia research at NIH, especially studying the use of hypothermia in surgery. He introduced the CO2 electrode and the first blood gas analysis system. In 1958, he joined UCSF in the Cardiovascular Research Institute and a new anesthesia department. In 1964 on sabbatical in Copenhagen, Severinghaus designed a blood gas slide rule relating oxygen pressure to hemoglobin saturation, and solving acid base and altitude problems. With help of many colleagues he published the standard human oxygen dissociation curve, with a simple equation, and accurate corrections for temperature and pH effects. His most visible contribution to respiratory care, however, was the development of the CO2 electrode which bears his name and is still in use today.
John Severinghaus has held an NIH Research Career Award from 1963 to 1991. His 350+ publications concern physiology of respiration and pulmonary and cerebral circulation, location of the medullary ventral surface CO2 chemoreceptors, physiologic effects of anesthetics, of high and low Pco2 and Po2, of high altitude on natives and newcomers on the lung, on cerebral blood flow, brain acid base balance and respiratory control. He developed and tested instruments such as pulse oximeters, brain and transcutaneous blood gas electrodes, introduced multiplexed mass spectrometry for multi-patient monitoring in surgery and through this, pioneered the introduction of computers in clinical anesthesia.
He served as NIH liason to the National Research Council of the National Academy of Science (1953-58), as member of an NIH study section (1961-66), and as respiration section editor of the Journal of Applied Physiology (1964-66). He continues to serve as referee for physiology, medicine and anesthesia journals.
He was named UCSF Faculty Research Lecturer in 1981, and received the first American Society of Anesthesiologists Award for Excellence in Research in 1986. He is an honorary Fellow of the Royal College of Anaesthetists (UK) (1989), and Doctor of Medicine Honoris Causa of the University of Copenhagen (1979). Severinghaus continues research at UCSF, with interests in the biochemical causes of high altitude cerebral edema, the theory of the limits of oxygen delivery to muscle cytochrome during maximum work, methods of testing human hypoxia responses, and instrumentation in anesthesia.
From 1953-1958, he was chief of anesthesia research at NIH, especially studying the use of hypothermia in surgery. He introduced the CO2 electrode and the first blood gas analysis system. In 1958, he joined UCSF in the Cardiovascular Research Institute and a new anesthesia department. In 1964 on sabbatical in Copenhagen, Severinghaus designed a blood gas slide rule relating oxygen pressure to hemoglobin saturation, and solving acid base and altitude problems. With help of many colleagues he published the standard human oxygen dissociation curve, with a simple equation, and accurate corrections for temperature and pH effects. His most visible contribution to respiratory care, however, was the development of the CO2 electrode which bears his name and is still in use today.
John Severinghaus has held an NIH Research Career Award from 1963 to 1991. His 350+ publications concern physiology of respiration and pulmonary and cerebral circulation, location of the medullary ventral surface CO2 chemoreceptors, physiologic effects of anesthetics, of high and low Pco2 and Po2, of high altitude on natives and newcomers on the lung, on cerebral blood flow, brain acid base balance and respiratory control. He developed and tested instruments such as pulse oximeters, brain and transcutaneous blood gas electrodes, introduced multiplexed mass spectrometry for multi-patient monitoring in surgery and through this, pioneered the introduction of computers in clinical anesthesia.
He served as NIH liason to the National Research Council of the National Academy of Science (1953-58), as member of an NIH study section (1961-66), and as respiration section editor of the Journal of Applied Physiology (1964-66). He continues to serve as referee for physiology, medicine and anesthesia journals.
He was named UCSF Faculty Research Lecturer in 1981, and received the first American Society of Anesthesiologists Award for Excellence in Research in 1986. He is an honorary Fellow of the Royal College of Anaesthetists (UK) (1989), and Doctor of Medicine Honoris Causa of the University of Copenhagen (1979). Severinghaus continues research at UCSF, with interests in the biochemical causes of high altitude cerebral edema, the theory of the limits of oxygen delivery to muscle cytochrome during maximum work, methods of testing human hypoxia responses, and instrumentation in anesthesia.


Class of 2020 Legends
Three outstanding individuals have been selected for the Class of 2020 Legends: Alvan L. Barach, MD, Robert M. Kacmarek, PhD, RRT, FAARC, and Neil R. MacIntyre, MD, FAARC.


Alvan L. Barach, MD
Alvan Leroy Barach, MD (1895–1977) made important contributions to Pulmonary Rehab and Oxygen Therapy. He turned the oxygen tent into a closed system, introduced portable O2 and authored the first report concerning supplemental oxygen and pneumonia. He recommended increasing periods of exercise for emphysema and patients on O2.
He wrote 4 books, authored more than 300 articles for professional journals, and wrote a novel "The Spectacle of Man". In 1956 his textbook "Pulmonary Emphysema" was published.
In 1950, he was one of three a contributors to the first minimum standards for Inhalation Therapy training programs. He served on the Board of Advisors (BOMA's predecessor).
Dr. Barach was awarded the first Honorary membership in our Association.
He wrote 4 books, authored more than 300 articles for professional journals, and wrote a novel "The Spectacle of Man". In 1956 his textbook "Pulmonary Emphysema" was published.
In 1950, he was one of three a contributors to the first minimum standards for Inhalation Therapy training programs. He served on the Board of Advisors (BOMA's predecessor).
Dr. Barach was awarded the first Honorary membership in our Association.

Robert M. Kacmarek, PhD, RRT, FAARC
Robert Kacmarek was an educator, manager and researcher. He authored or co-authored over 300 articles indexed in PubMed. He authored 19 textbooks and lectured over 700 hundred times nationally and internationally. Bob was a principal investigator of a number of multicenter trials for the treatment of ARDS and application of mechanical ventilation with emphasis on PEEP.
Bob was the first RT to receive full professorship in an American medical school (Harvard). He worked with physicians around the world, establishing a bench and animal laboratory in the Department of Anesthesiology at Massachusetts General Hospital. He mentored pulmonary and anesthesiology physician, fellows and RTs from the US, Asia, Europe and the Middle East.
His lasting accomplishments include research papers in journals primarily for physicians and lecturing at international meetings presenting original research. His presence at these meetings brought recognition to the profession and elevated the status of respiratory therapist around the world. He won numerous awards from physician organizations and the AARC. He served on the editorial boards of CCM, RESPIRATORY CARE, and Intensive Care Medicine(ICM).
Bob was also the first RT Director to require all his employees to be RRTs. The profession has been enhanced by his vision to push educational and professional standards.
Dr. Kacmarek was awarded FAARC in 1998, received the AARC's Jimmy A Young Medal in 2008, and received AARC Life Membership in 2021.
Bob was the first RT to receive full professorship in an American medical school (Harvard). He worked with physicians around the world, establishing a bench and animal laboratory in the Department of Anesthesiology at Massachusetts General Hospital. He mentored pulmonary and anesthesiology physician, fellows and RTs from the US, Asia, Europe and the Middle East.
His lasting accomplishments include research papers in journals primarily for physicians and lecturing at international meetings presenting original research. His presence at these meetings brought recognition to the profession and elevated the status of respiratory therapist around the world. He won numerous awards from physician organizations and the AARC. He served on the editorial boards of CCM, RESPIRATORY CARE, and Intensive Care Medicine(ICM).
Bob was also the first RT Director to require all his employees to be RRTs. The profession has been enhanced by his vision to push educational and professional standards.


Neil R. MacIntyre, MD, FAARC
Neil MacIntyre is known as a researcher, educator and mentor. He has been the Medical Director of the RC Department, PF Lab and Pulmonary Rehab at Duke University since 1981 and Professor of Medicine at Duke since 1995. He is a Fellow of the ACCP,ACCPVR and AARC.
He has held offices with the ATS,ALA,NAMDRC, Allergy and Asthma, and AACPR. He has authored or co-authored over 100 scientific articles, 80 books and 80 abstracts.
He has chaired AARC Consensus Conferences, served on the RC Journal Editorial Board since 1988, served as Vice Chair of the ARCF since 1992, and served 14 years on BOMA as a member and several terms as Chair.
Dr. MacIntyre has delivered hundreds of presentations at AARC International Congresses. He was awarded honorary membership in the AARC and is a recipient of the Jimmy A. Young Medal, AARC's highest award.
He has held offices with the ATS,ALA,NAMDRC, Allergy and Asthma, and AACPR. He has authored or co-authored over 100 scientific articles, 80 books and 80 abstracts.
He has chaired AARC Consensus Conferences, served on the RC Journal Editorial Board since 1988, served as Vice Chair of the ARCF since 1992, and served 14 years on BOMA as a member and several terms as Chair.
Dr. MacIntyre has delivered hundreds of presentations at AARC International Congresses. He was awarded honorary membership in the AARC and is a recipient of the Jimmy A. Young Medal, AARC's highest award.


Class of 2021 Legends
The three Legends in the Class of 2021 include Robert Chatburn, Gary Smith, and Barry A. Shapiro, MD


Robert Chatburn, MHHS, RRT-NPS, FAARC
Rob Chatburn has a number of significant accomplishments in respiratory care which include
undergraduate and graduate degrees in respiratory therapy, electrical engineering and health sciences; professor, department of medicine, Lerner College of Medicine of Case Western Reserve University; prolific researcher; author of >150 peer reviewed scientific papers and >250 abstracts; author, editor or co-editor of 16 textbooks/journal volumes and 52 textbook chapters; inventor, holding two US patents for mechanical ventilation; co-designer of AARC Benchmarking project and website; author of Research track of the AARC Leadership Institute; designer of the taxonomy for modes of mechanical ventilation; and myriad of academic presentations at major respiratory and pulmonary conferences around the world.


Gary Smith, RRT (Hon), FAARC
Gary Smith first earned his Certified Respiratory Therapist credential in 1971 and went on to work as the Director of Respiratory Care at several different hospitals in Georgia. In addition, he was a Clinical Instructor at Macon Hospital in Macon, GA. Gary became a member of the NBRC Board of Trustees in 1979 and served as President of the NBRC in 1982 and 1983. He then went on to join the staff at the NBRC in 1983 and was the Associate Executive Director from 1986-2001 before he became the Chief Executive Officer in 2002. Gary retired from the National Board for Respiratory Care after serving in the CEO position for 16 years.
Gary is a former Chairman of the National Commission for Certifying Agencies (NCCA) and Past President of the National Organization for Competency Assurance (NOCA). In addition to his duties with the NBRC and AMP, Gary served as Secretary/Treasurer of the American Respiratory Care Foundation from 1996 until 2018.
Gary received the ICRC Toshihiko Koga Medal, MD in 2010 and was honored as a National Honorary Member of the Lambda Beta Society in 1998. He is also the editor of the book "Respiratory Care – Evolution of a Profession".
Gary is a former Chairman of the National Commission for Certifying Agencies (NCCA) and Past President of the National Organization for Competency Assurance (NOCA). In addition to his duties with the NBRC and AMP, Gary served as Secretary/Treasurer of the American Respiratory Care Foundation from 1996 until 2018.
Gary received the ICRC Toshihiko Koga Medal, MD in 2010 and was honored as a National Honorary Member of the Lambda Beta Society in 1998. He is also the editor of the book "Respiratory Care – Evolution of a Profession".


Barry A. Shapiro, MD
Barry Shapiro, MD was a leader in critical medicine and blood gas technology. He practiced at Northwestern University School of Medicine for over 30 years. He authored and co-authored several textbooks for RC including "Clinical Application of Blood Gases" in 1973, "Clinical Application of RC" and "Foundation of RT Services". He co-authored "Case Studies in Critical Care Medicine" and the "Yearbook of Critical Medicine" (1996, 1997 and 1998.)
He was an oral examiner for the NBRC. Dr. Shapiro was an advocate for respiratory therapists and lectured at affiliate, national and international meetings for respiratory care. In 1997, he was chosen as the first presenter for the Program Committee's Special Lecture. He was awarded Honorary membership in the AARC and was a Jimmy A. Young Medalist.
He also was active in the Society of Critical Care Medicine(SCCM) and has an award named for him for Excellence in Critical Care Medicine.
He was an oral examiner for the NBRC. Dr. Shapiro was an advocate for respiratory therapists and lectured at affiliate, national and international meetings for respiratory care. In 1997, he was chosen as the first presenter for the Program Committee's Special Lecture. He was awarded Honorary membership in the AARC and was a Jimmy A. Young Medalist.
He also was active in the Society of Critical Care Medicine(SCCM) and has an award named for him for Excellence in Critical Care Medicine.


Class of 2022 Legends
Five Legends were designated in 2022.

Thomas Barnes, EdD, RRT, FAARC
Dr. Thomas Barnes has been strong advocate for respiratory therapy education throughout his career. He is the author of 5 textbooks, 16 book chapters, 30 published articles and 30 research abstracts. He was the primary author of AARC's "2015 and Beyond."
Early in his career, he served as the 1971 Speaker of the AARC House of Delegates. He served as AARC President in 1977. Dr. Barnes received the Bird Literary Award in 1975 and 1979. was awarded AARC Life membership in 1985, received the Jimmy A Young Medal in 1997, was designated an AARC Fellow (FAARC) in 1999, was designated Lambda Beta Society's national honorary member in 2001, was named AARC Education Section's Practitioner of the Year in 2010, and received life membership in the Coalition for Baccalaureate and Graduate Respiratory Therapy Education in 2018.
Dr. Barnes received an “Award for Excellence in Medical Publications” in the 1989 Book Competition from the American Medical Writers Association for his textbook Respiratory Care Practice.
Dr. Barnes was a tenured Full Professor for the Bachelor of Science degree Cardiopulmonary Sciences program at Northeastern University that he established in 1976. He moved to emeritus status at Northeastern in 2005. He was lead faculty for the Northeastern University Master of Science in Respiratory Care Leadership program that he established from 2008-2023.
Early in his career, he served as the 1971 Speaker of the AARC House of Delegates. He served as AARC President in 1977. Dr. Barnes received the Bird Literary Award in 1975 and 1979. was awarded AARC Life membership in 1985, received the Jimmy A Young Medal in 1997, was designated an AARC Fellow (FAARC) in 1999, was designated Lambda Beta Society's national honorary member in 2001, was named AARC Education Section's Practitioner of the Year in 2010, and received life membership in the Coalition for Baccalaureate and Graduate Respiratory Therapy Education in 2018.
Dr. Barnes received an “Award for Excellence in Medical Publications” in the 1989 Book Competition from the American Medical Writers Association for his textbook Respiratory Care Practice.
Dr. Barnes was a tenured Full Professor for the Bachelor of Science degree Cardiopulmonary Sciences program at Northeastern University that he established in 1976. He moved to emeritus status at Northeastern in 2005. He was lead faculty for the Northeastern University Master of Science in Respiratory Care Leadership program that he established from 2008-2023.


Jeremiah Mead, MD
Dr. Jeremiah “Jere” Mead (1920-2009) had a profound influence on the profession of Respiratory Care. He established an entirely new field of research; pulmonary mechanics. He created, developed, nurtured, and maintained this field during his 37-year career at Harvard School of Public Health where he was the first Cecil K. and Philip Drinker Professor of Environmental Physiology, appointed in 1976.
Dr. Mead was a tinkerer who frequently built conceptual models out of household items, and embraced seemingly outlandish questions and hypotheses as the essential driving force of innovation. Mead’s interest in decoding the normal mechanisms of breathing inspired the growth of the new field of respiratory mechanics, which continued to expand throughout the latter half of the twentieth century. He and his collaborators developed methods and instruments for measuring airflow and evaluating pulmonary function with ever-increasing accuracy. He is considered the inventor of modern spirometry as used in PFTs labs around the world.
Perhaps his most recognized discovery came in the late ‘50s with then-research fellow Mary Ellen Avery. Mead and Avery showed that fatal respiratory distress syndrome in newborns was caused by abnormal surface tension in the lungs. Their discovery led to the development of surfactant replacement therapy, a treatment that continues to save newborn lives. Jere Mead is a giant on the field of respiratory physiology and a true legend.
Dr. Mead was a tinkerer who frequently built conceptual models out of household items, and embraced seemingly outlandish questions and hypotheses as the essential driving force of innovation. Mead’s interest in decoding the normal mechanisms of breathing inspired the growth of the new field of respiratory mechanics, which continued to expand throughout the latter half of the twentieth century. He and his collaborators developed methods and instruments for measuring airflow and evaluating pulmonary function with ever-increasing accuracy. He is considered the inventor of modern spirometry as used in PFTs labs around the world.
Perhaps his most recognized discovery came in the late ‘50s with then-research fellow Mary Ellen Avery. Mead and Avery showed that fatal respiratory distress syndrome in newborns was caused by abnormal surface tension in the lungs. Their discovery led to the development of surfactant replacement therapy, a treatment that continues to save newborn lives. Jere Mead is a giant on the field of respiratory physiology and a true legend.
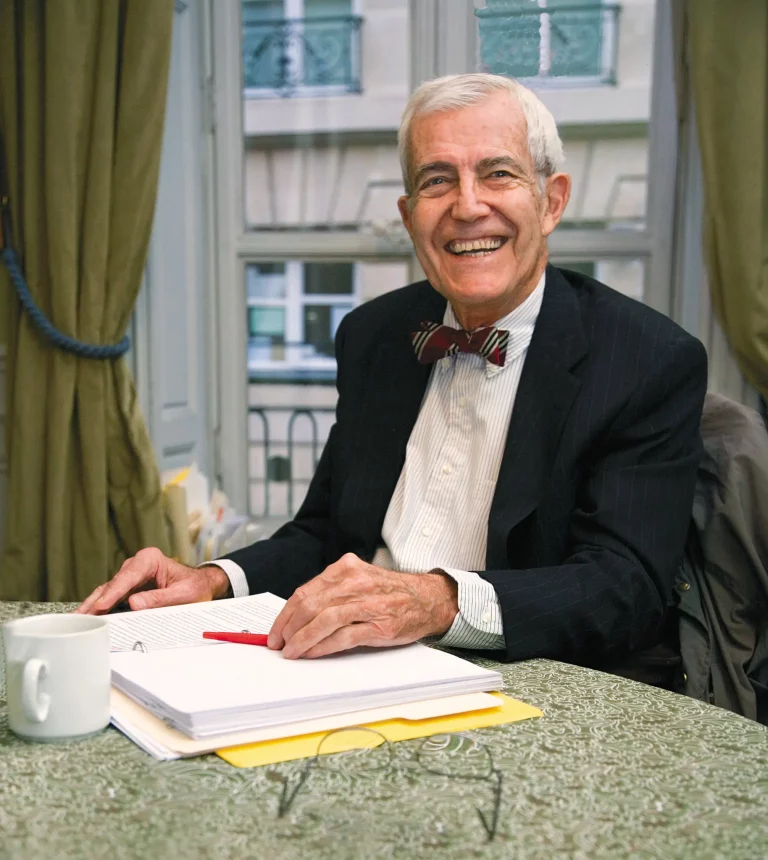
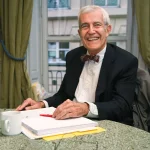
John Murray, MD
John Murray, MD (1928-2020) was a world renowned pulmonary physician and physiologist. He was tirelessly dedicated to what was then called San Francisco General Hospital (now, Zuckerberg San Francisco General Hospital & Trauma Center), where he was chief of pulmonology from 1966 until 1989. He arrived at a time when the hospital was being fully integrated into UCSF training programs, and he was a key figure in the successful partnership. In addition, he served as chief of the medical staff and conducted a successful research program, focused mainly on the pathogenesis and treatment of acute lung injury/ARDS. Long after retiring in 1994, he continued to serve as an attending physician in the MICU, teaching and inspiring both physicians and respiratory therapists to value concern for the patient, above all. Dr. Murray left indelible marks on the clinical practice of pulmonary medicine, the process of selecting and training fellows in pulmonary disease, and on lung disease research. Moreover, he played an instrumental role in the evolution of the American Thoracic Society into the strong, internationally respected professional society it is today. The breadth of his achievements serves as a reflection of his talents for clear thinking, clear writing and clear speaking. He helped to create the field of pulmonology itself, establish its national society and guide its journal, and design its training programs and NHLBI research support. His classic books, "The Normal Lung" and "The Abnormal Lung" are classic works fundamental to the respiratory care community.


Jerome Sullivan, PhD, RRT, FAARC
Jerome Sullivan served as Program Director and Dean of the RC bachelor's degree program at The Toledo State University for 36 years. He become Professor Emeritus in 2009. He served as President of the Ohio Society for Respiratory Therapy in 1976 and 77. He served on the Board of the NBRC in 1989. He was President of the AARC in 1990. He also served as Secretary and on numerous committees. As President, Jerome established the first Clinical Practice Guidelines Committee, the International Fellows Program and was the first President of the International Council in 1991 He served as the International Council President until 2020.
In 1993 he was appointed to help establish the new accreditation program(CoARC) for the AARC, which became reality in 1997. Jerome has received numerous awards and honors including;The Jimmy A Young Medal,AARC Fellow,ARCF Hector Leon Garza International Award,ICRC Toshihiko Koga MD Medal and the ARCF established the Jerome Sullivan Research Fund.
Jerome's desire to assist international education is evident as he chaired the International Education Recognition System(IERS) which provides formal recognition for RC programs, seminars and schools around the world. He discussed the project in an article published in the Journal of the Japan Society for Respiratory Care Rehabilitation. Recently he spearheaded, along with Hassan Alorainy, the Fundamental RC Support Course(FRCSC) due to launch in 2022. This is a modular training course with 38 chapters written by RTs and physicians. International instructors will receive training to deliver the FRCSC courses in their nations. No other individual has had a greater impact on international RC than Jerome Sullivan.
In 1993 he was appointed to help establish the new accreditation program(CoARC) for the AARC, which became reality in 1997. Jerome has received numerous awards and honors including;The Jimmy A Young Medal,AARC Fellow,ARCF Hector Leon Garza International Award,ICRC Toshihiko Koga MD Medal and the ARCF established the Jerome Sullivan Research Fund.
Jerome's desire to assist international education is evident as he chaired the International Education Recognition System(IERS) which provides formal recognition for RC programs, seminars and schools around the world. He discussed the project in an article published in the Journal of the Japan Society for Respiratory Care Rehabilitation. Recently he spearheaded, along with Hassan Alorainy, the Fundamental RC Support Course(FRCSC) due to launch in 2022. This is a modular training course with 38 chapters written by RTs and physicians. International instructors will receive training to deliver the FRCSC courses in their nations. No other individual has had a greater impact on international RC than Jerome Sullivan.


John B. West, MD
John West, MD, PhD is a respiratory physiologist who made major research contributions in many areas of respiratory physiology that have had profound effects of the practice of respiratory care. Chief among these is the understanding of ventilation-perfusion relationships in the lung. He is also widely known for leading the medical research expedition to Mount Everest in 1981, which investigated the influence of altitude and exertion on human physiology. Since it was first published in 1974, his book, "Respiratory Physiology: the Essentials" (Lippincott, Williams & Wilkins) has become the most widely used introductory text in respiratory physiology and respiratory care. It has been translated into at least 17 languages.
He was a member of the NIH Cardiovascular and Pulmonary Study Section from 1971–1975, and chairman from 1973–1975; a member of the Physiology Committee of the National Board of Medical Examiners (1973–1976); and a member of the Cardiopulmonary Council of AHA (1977–78).After election to membership in American Physiological Society in 1970 and to Council in 1981, in 1983 he became president elect, and became the 57th APS President for 1984-85. For NASA he has been chairman of the Science Verification Committee for Spacelab in 1983 and a member of their Advisory Committee on Scientific Uses of Space Station in 1984. Also in that year he served as a member of a NASA Committee on Space Biology.
He was a member of the NIH Cardiovascular and Pulmonary Study Section from 1971–1975, and chairman from 1973–1975; a member of the Physiology Committee of the National Board of Medical Examiners (1973–1976); and a member of the Cardiopulmonary Council of AHA (1977–78).After election to membership in American Physiological Society in 1970 and to Council in 1981, in 1983 he became president elect, and became the 57th APS President for 1984-85. For NASA he has been chairman of the Science Verification Committee for Spacelab in 1983 and a member of their Advisory Committee on Scientific Uses of Space Station in 1984. Also in that year he served as a member of a NASA Committee on Space Biology.


Future Legends?
The Boards of the AARC, CoARC, NBRC, and ARCF may submit up to five nominees each year to the Legends of Respiratory Care Selection Committee.
If you have an individual you'd recommend be nominated as a Legend of Respiratory Care, contact the appropriate Board with your justification outlining the individual's accomplishments and significant historic contributions to our profession.
If you have an individual you'd recommend be nominated as a Legend of Respiratory Care, contact the appropriate Board with your justification outlining the individual's accomplishments and significant historic contributions to our profession.


Class of 2023 Legends
Three individuals were designated as Legends of Respiratory Care in 2023.


Robert A. Balk, MD, MACP, MCCM, FCCP, FAARC
Dr. Balk received his medical degree from University of Missouri-Kansas City School of Medicine in 1978 and has been in practice for more than 20 years. Throughout his career, Bob taught at the University of Arkansas for Medical Sciences and Rush University Medical Center and has been recognized for numerous awards including his outstanding contributions in critical care medicine and Cystic Fibrosis and ECMO care.
Dr. Balk joined the NBRC Board of Trustees in 2010 after first serving as a consultant in 2009. During his time on the board, Dr. Balk has served on numerous committees but most notably was instrumental in the development of the Adult Critical Care Specialty Examination which was implemented in 2012. Bob is the consummate professional, volunteer and a true champion of the respiratory care profession. He has over 150 original peer reviewed manuscripts and research publications, has given hundreds of lectures and contributed 42 chapters in books. Bob has also published over 100 abstracts and contributed to editing more than 70 publications.
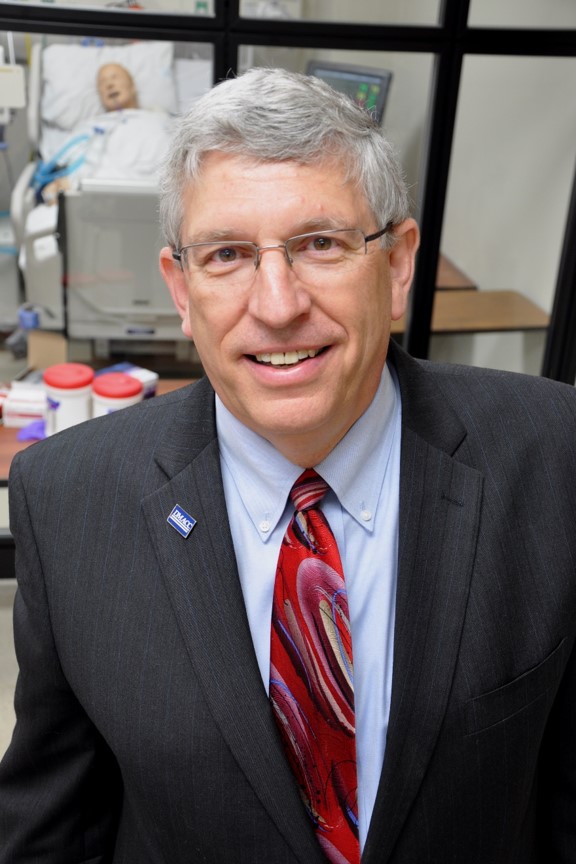

Kerry E. George, MEd, RRT, RRT-ACCS, RRT-SDS, FAARC
Kerry began his career as an on-the-job trainee at Freeport Memorial Hospital in Freeport Illinois in the summer of 1973. In 1974 he attended the accelerated respiratory therapy program at the University of Chicago Hospital and Clinics School. In 1975 he began working at St. Mary’s Medical Center as a staff therapist and earned his RRT credential in November of 1975. While working at St. Mary’s, Kerry decided there were some changes in the education of new therapists that were needed and decided to become involved in the education of new respiratory therapists. Becoming a Program Director of the Des Moines Area Community College Respiratory Therapy program in the summer 1977 helped him do just that in a position that he held for over 40 years.
Throughout his career, Kerry served in many volunteer roles within the profession, including President of the AARC in 1997 and then joining the NBRC Board of Trustees in 2003 where he has contributed beyond measure to the credentialing system by serving on numerous examination and standing committees and President of the NBRC Board in 2012 and 2013. He was a member of the NBRC’s subsidiary, AMP, Board of Directors from 2008-2015. Kerry joined the Lambda Beta Executive Board in 1998. He served as president from 2016-2018. In addition, he also served on numerous respiratory care boards and often in leadership positions: IA Board for Respiratory Care, IL Society for Respiratory Care, WI Society for Respiratory Care, IA Society for Respiratory Care, American Lung Association of IA, Commission on Accreditation of Allied Health Education Programs, National Health Data Collaborative, and Health Professions Network.
Kerry has been an RT for 47 years and has been instrumental in mentoring his students and colleagues to achieve leadership positions as they advance in their careers. His commitment and dedication to the credentialing system is unmatched.


Henning Pontoppidan, MD
Henning Pontoppidan, MD, was a pioneer in the field of pulmonary intensive care and anesthesia. He passed away on October 20, 2017 at the age of 92.
In 1961, he established the first respiratory intensive care unit in the country at Mass General. The Respiratory Intensive Care Unit (RICU) became a model for hospitals throughout the world.
Colleagues remember Dr. Pontoppidan warmly for his extraordinary intuition, wisdom and great kindness. He spent long hours with residents, fellows, medical students, nurses and respiratory therapists selflessly imparting his wisdom to the
next generation of intensivists. Dr. Pontoppidan had an enormous influence on intensive care worldwide through his personal and professional relationships and his publications.
Dr. Pontoppidan with his many international fellows studied the use of positive end-expiratory pressure ventilation in acute respiratory failure, and synthesized the entire field of acute respiratory care. In 1965, together with MGH Drs. H. Bendixen, L. Egbert, J. Hedley-Whyte and M Laver, he published "Respiratory Care", which became known as the “red bible,” after the color of the cover, the first textbook in the field of respiratory intensive care. He then worked to assure dissemination of this knowledge, running the first continuing education respiratory and critical care course given annually through Harvard Medical School in 1973. The course attracted large groups of US and international physicians, nurses and therapists to Boston and continued for many years despite the rising competition. He also published a subsequent textbook in 1973 with Drs. Bennie Geffin and Edward Lowenstein entitled "Acute Respiratory Failure in the Adult."
In 1988, Dr. Pontoppidan became the first Reginald Jenney Professor of Anesthesia at Harvard Medical School and Mass General, a chair endowed by one of his grateful patients. In 2011, on the hospital’s bicentennial, Dr. Pontoppidan’s
accomplishments were recognized with the establishment of the Henning Pontoppidan Visiting Professorship.