COVID-19 and the Respiratory Therapist
Here we take a look at the RTs fighting COVID-19 and the impact the pandemic had on them in 2020. RTs were on the front lines, caring for patients, preparing new RTs to join the fight and helping their friends and neighbors deal with the devastating impact this pandemic has had on all.


Pandemic Overview
The COVID-19 pandemic, also known as the coronavirus pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) became a global pandemic and threat to health worldwide with its first beginnings documented in 2019 and spreading worldwide in the beginning of 2020. This gallery will focus on the first year of the pandemic.
The outbreak was first identified in Wuhan, China, in December 2019. The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern on January 30, 2020, and a pandemic on March 11, 2020.
Little did anyone at the time understand at its onset the effect it would have globally. What followed was a series of shortages in the health care arena including: personal protective equipment (PPE), shortages and threats of shortages of hospital beds, ICU beds, ventilators, and respiratory therapists.
In the United States and throughout the world, stay at home and shelter in place orders led to a shutdown of the economy and life as usual. Universities, businesses (other than those deemed essential), and a vast array of stores and service providers were forced to either close or conduct business in a virtual world.
Wearing masks and social distancing became the norm. Shortages of other goods occurred either due to hoarding, increased demand, or disruptions to the supply chain. These included shortages of meat, toilet paper, hand sanitizer, and surgical masks.
Seamstresses were called to duty to sew cotton masks in lieu of the shortage of surgical masks to try and meet the demand for health care workers as well as other front-line and essential workers, and finally to anyone venturing out into public places.
What follows is how a virus first identified in Wuhan China, became a pandemic, a worldwide threat to the health and economic wellbeing of those around the world and how respiratory therapists responded as on the frontlines caring for those affected—becoming the “unsung heroes” of the pandemic crisis.
The outbreak was first identified in Wuhan, China, in December 2019. The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern on January 30, 2020, and a pandemic on March 11, 2020.
Little did anyone at the time understand at its onset the effect it would have globally. What followed was a series of shortages in the health care arena including: personal protective equipment (PPE), shortages and threats of shortages of hospital beds, ICU beds, ventilators, and respiratory therapists.
In the United States and throughout the world, stay at home and shelter in place orders led to a shutdown of the economy and life as usual. Universities, businesses (other than those deemed essential), and a vast array of stores and service providers were forced to either close or conduct business in a virtual world.
Wearing masks and social distancing became the norm. Shortages of other goods occurred either due to hoarding, increased demand, or disruptions to the supply chain. These included shortages of meat, toilet paper, hand sanitizer, and surgical masks.
Seamstresses were called to duty to sew cotton masks in lieu of the shortage of surgical masks to try and meet the demand for health care workers as well as other front-line and essential workers, and finally to anyone venturing out into public places.
What follows is how a virus first identified in Wuhan China, became a pandemic, a worldwide threat to the health and economic wellbeing of those around the world and how respiratory therapists responded as on the frontlines caring for those affected—becoming the “unsung heroes” of the pandemic crisis.


First Reported Cases in China
On December 31, 2019, the Wuhan Municipal Health Commission, China reported a cluster of cases of pneumonia in Wuhan, Hubei Province. A novel coronavirus was eventually identified.
World Health Organization Reports Pneumonia Cluster
On January 4, 2020, the World Health Organization (WHO) reported on social media that there was a cluster of pneumonia cases – with no deaths – in Wuhan, Hubei province.
WHO Guidelines Issued
On January 10, 2020, WHO issued guidelines to all countries on how to detect, test and manage potential cases, based on what was known about the virus at the time. Based on experience with SARS and MERS, infection and prevention control guidance were published to protect health care workers recommending droplet and contact precautions when caring for patients, and airborne precautions for aerosol generating procedures conducted by health care workers.
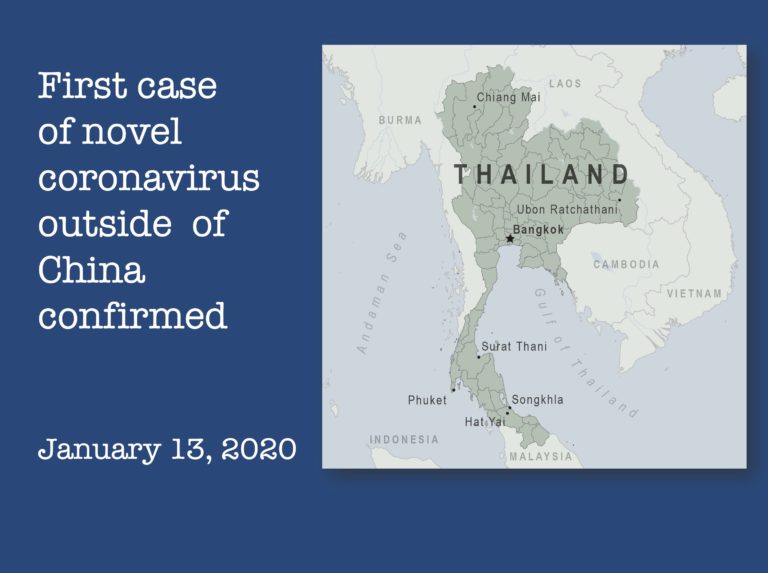
Confirmed Case in Thailand
On January 13, 2020, Thailand's Ministry of Public Health confirm a case of COVID-19 in Thailand, the first recorded case of the novel coronavirus outside of China.
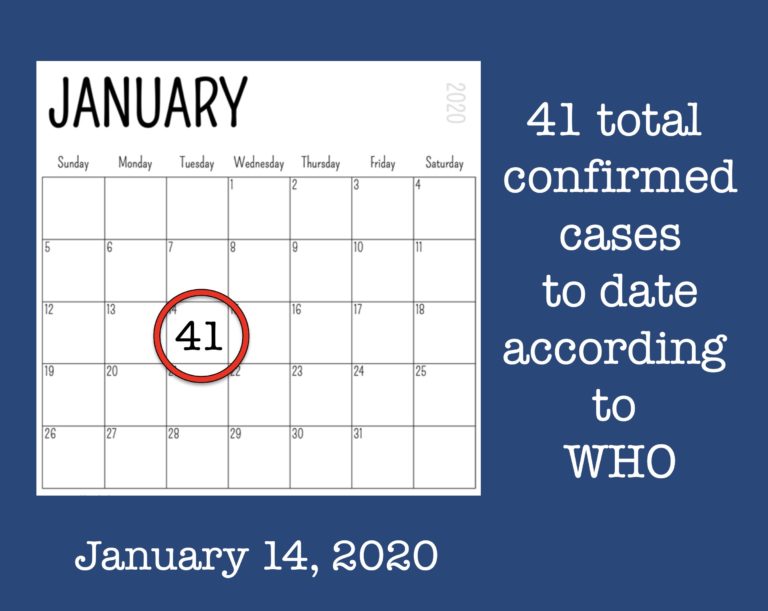
41 Confirmed Cases
On January 14, 2020, WHO issued a briefing that there may have been limited human-to-human transmission of the coronavirus (in the 41 confirmed cases), mainly through family members, and that there was a risk of a possible wider outbreak. WHO also surmised that human-to-human transmission would not be out of the question given previous experience with SARS, MERS and other respiratory pathogens.
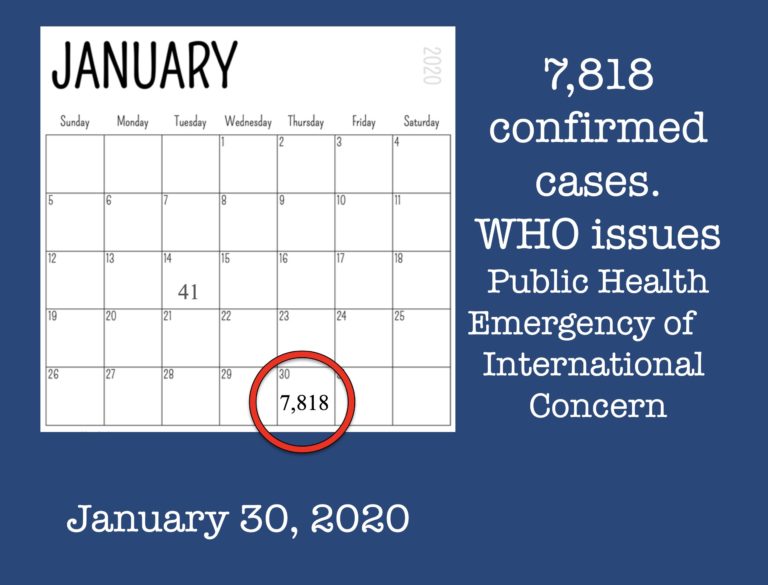

WHO Reports 7,818 Cases
On January 30, 2020, WHO advised that the outbreak constituted a Public Health Emergency of International Concern (PHEIC) and declared the novel coronavirus outbreak (2019-nCoV) a PHEIC.
WHO reported 7818 total confirmed cases worldwide, with the majority of these in China, and 82 cases reported in 18 countries outside China. WHO gave a risk assessment of very high for China, and high at the global level.
WHO reported 7818 total confirmed cases worldwide, with the majority of these in China, and 82 cases reported in 18 countries outside China. WHO gave a risk assessment of very high for China, and high at the global level.
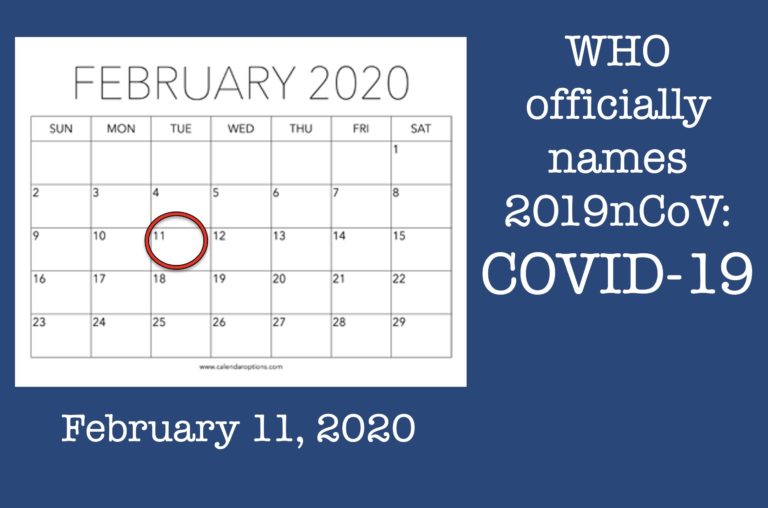

WHO Names COVID-19
On February 11, 2020, the World Health Organization announced that the coronavirus disease referenced as 2019nCoV would officially be designated COVID-19.
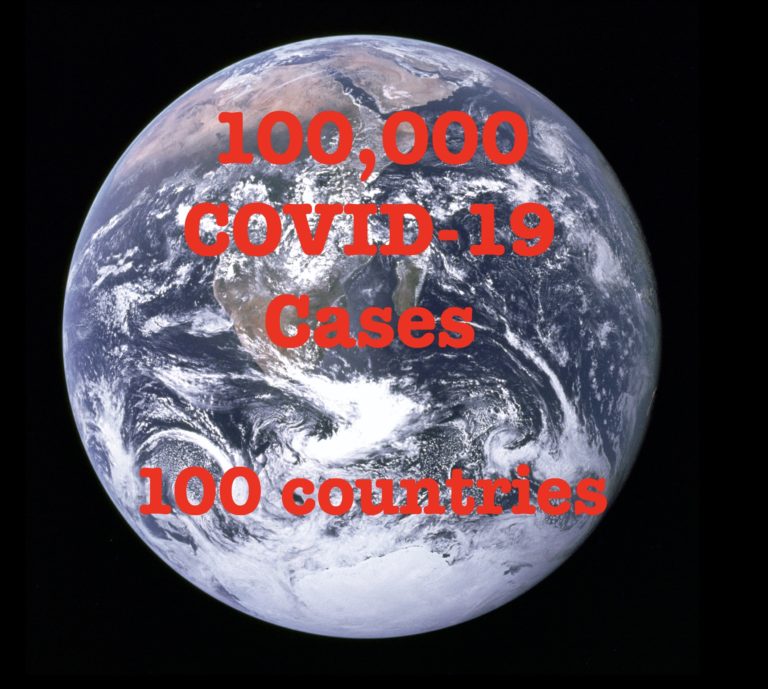
100,000 Cases Globally
On March 8, 2020, the World Health Organization announced the total number of cases from the 100 countries that reported COVID-19 cases had reached 100,000.
COVID-19 Declared A Pandemic
The World Health Organization declared COVID-19 a pandemic on March 11, 2020.

Previous Pandemics and Epidemics
Although much media attention has been given to COVID-19, this isn’t the first pandemic or epidemic in our history. A few notable pandemics/epidemics that have made notable history include the Black Death (1346-1353), Flu Pandemic (1889-1890) in which approximately 1 million persons perished, the Polio epidemic (1916-1954) which wasn’t abolished until the development of the vaccine in 1954 by Dr. Salk, and the Spanish Flu (1918-1920) in which there were reported to be 500 million victims.
Click on this link to read more about the worst epidemics and pandemics in history in this March 20, 2020 article in LiveScience.
Also, noteworthy is the role of the inhalation therapist (respiratory therapist) in the care and management of those patients falling victim to polio during the 1940s and 1950s, as polio led to respiratory failure as well, although by an entirely different route.
Click on this link to read about the transition from iron lungs to positive pressure ventilation and the creation of intensive care units.
Click on this link to read more about the worst epidemics and pandemics in history in this March 20, 2020 article in LiveScience.
Also, noteworthy is the role of the inhalation therapist (respiratory therapist) in the care and management of those patients falling victim to polio during the 1940s and 1950s, as polio led to respiratory failure as well, although by an entirely different route.
Click on this link to read about the transition from iron lungs to positive pressure ventilation and the creation of intensive care units.
Coronaviruses
Coronaviruses are named for the crown-like spikes on their surface. There are seven coronaviruses that can infect people, including: MERS-CoV (the beta coronavirus that causes Middle East Respiratory Syndrome, or MERS); SARS-CoV (the beta coronavirus that causes severe acute respiratory syndrome, or SARS); SARS-CoV-2 (the novel coronavirus that causes coronavirus disease 2019, or COVID-19).
Click on this link for more information from the CDC.
How do SARS and MERS compare with COVID-19? Click on this link for more information.
Click on this link for more information from the CDC.
How do SARS and MERS compare with COVID-19? Click on this link for more information.


Stay Home Mandates
As COVID-19 cases increased across the country, "stay home" mandates were implemented in many parts of the country to attempt to contain the virus. Many Americans were forced to work from home while large numbers joined the ranks of the unemployed. In many communities, only businesses deemed essential were allowed to remain open.


Masks Required
While initially a recommendation, face masks soon became a mandate for customers and employees in indoor and outdoor businesses in many parts of the country.
With N95 masks and medical grade masks in short supply and reserved for frontline workers, the general public resorted to the use of simple cloth masks. Social media was flooded with patterns and tips for creating homemade masks and the use of alternative supplies, especially when elastic and cording for ear loops was suddenly in short supply.
Many complaints have been voiced about wearing a mask in a store for a short shopping trip. It's almost comical to watch shoppers rip off their masks the moment they exit a store. One can only hope they truly appreciate what respiratory therapists and other frontline workers endure for a 12 hour shift in their full PPE "armor".
With N95 masks and medical grade masks in short supply and reserved for frontline workers, the general public resorted to the use of simple cloth masks. Social media was flooded with patterns and tips for creating homemade masks and the use of alternative supplies, especially when elastic and cording for ear loops was suddenly in short supply.
Many complaints have been voiced about wearing a mask in a store for a short shopping trip. It's almost comical to watch shoppers rip off their masks the moment they exit a store. One can only hope they truly appreciate what respiratory therapists and other frontline workers endure for a 12 hour shift in their full PPE "armor".
Image from Connie VanGerpen


RT with PPE
One of the dedicated Respiratory Therapists at Presbyterian Brooklyn Methodist Hospital in New York City is shown in full PPE.
Image from Felix Khusid
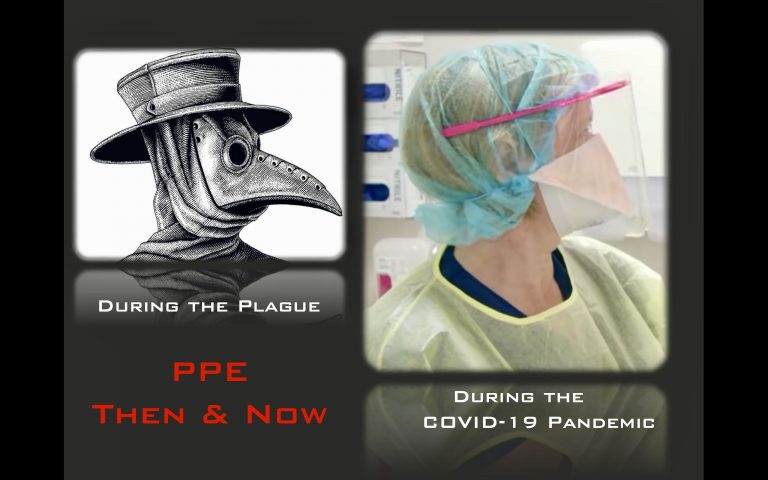

PPE During Pandemics
Personal protective equipment (PPE) used during pandemics centuries apart had basic similarities: head coverings, eye protection, and face masks.
During the plague, the beaks of the masks were filled with aromatic herbs.
During the plague, the beaks of the masks were filled with aromatic herbs.

Social Distancing
To reduce the spread of COVID-19, social (or physical) distancing, individuals were advised to maintain a distance of at least 6 feet from non-members of one's household in both indoor and outdoor spaces.
Grocery stores and other businesses implemented "one way" aisles to reduce contact between shoppers and placed floor markers to encourage social distances in areas where lines were expected, such as check out areas and customer service .
Grocery stores and other businesses implemented "one way" aisles to reduce contact between shoppers and placed floor markers to encourage social distances in areas where lines were expected, such as check out areas and customer service .
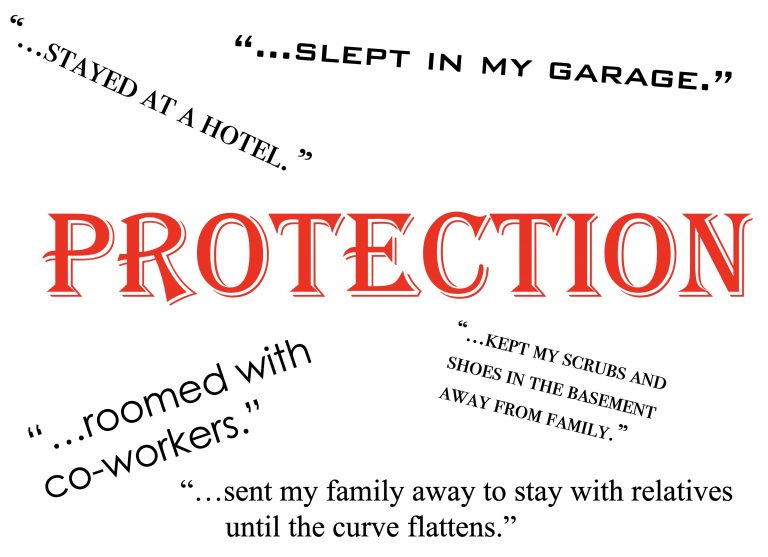
RTs Protect Household Members
After exposure to patients with confirmed cases of COVID-19, many Respiratory Therapists working on the frontlines implemented measures to protect the members of their household from possible exposure to the virus.
Some set up changing stations outdoors or in their garages to remove clothing and work-related items outside the living quarters. Some sent vulnerable family members to stay with relatives and friends to reduce possible exposure. Others set up tents or sleeping areas in garages, slept in campers or RVs, or confined themselves to basements, away from other members of the household. Some hotel chains offered hotel rooms to frontline workers at significantly reduced costs while some companies reimbursed their frontline workers for their alternate housing expenses.


Clear Your Calendar
As the pandemic continued, difficult decisions were made to limit public events. Some state mandates initially limited the size of public gatherings to 10 or fewer while others allowed up to 50 at an event once the rate of COVID-19 cases was reduced in a community. As a result, many events were postponed indefinitely or cancelled. Many tournaments and sports seasons were cancelled or significantly modified. Weddings, funerals, graduation ceremonies were among the events subjected to the attendance restrictions resulting in postponement, restricted guest lists, or video streaming alternatives.
Due to the restrictions of crowd size imposed within communities and/or states, the general public was left with limited activities for entertainment outside the home.
Due to the restrictions of crowd size imposed within communities and/or states, the general public was left with limited activities for entertainment outside the home.
In-person Education Disrupted
As the world changed daily amid the pandemic, and closures disrupted personal lives and businesses and K-12 schools across the nation and the world, disruptions also affected universities and colleges across the country.
Since respiratory therapist programs are housed in these academic institutions, the training of respiratory therapist students was impacted as well. How to train respiratory therapist students when campuses converted to on-line learning? And what about clinical and laboratory courses? The spring semester proved to be unique for millions of college students nationwide as institutions struggled with the continued delivery of education in the on-line environment.
The University of Washington became the first large university in the U.S. to close related to the pandemic. The school canceled in-person classes for its nearly 50,000 students. Students converted to remote learning, taking classes and exams on-line. Soon after, schools across the country followed suit.
Harvard joins a growing number of colleges and universities that announced a major shift to remote learning canceling all in-person classes and, in some cases, asking students not to remain on campus. The trend of closing campus buildings, academic buildings, and dorms, sending students home, converting to on-line learning continues nationwide.
Click on this link for a March 2020 article regarding school shutdowns.
Click on this link to access an early March 2020 article listing colleges and universities that closed campuses and in-person classes due to the pandemic.
Since respiratory therapist programs are housed in these academic institutions, the training of respiratory therapist students was impacted as well. How to train respiratory therapist students when campuses converted to on-line learning? And what about clinical and laboratory courses? The spring semester proved to be unique for millions of college students nationwide as institutions struggled with the continued delivery of education in the on-line environment.
The University of Washington became the first large university in the U.S. to close related to the pandemic. The school canceled in-person classes for its nearly 50,000 students. Students converted to remote learning, taking classes and exams on-line. Soon after, schools across the country followed suit.
Harvard joins a growing number of colleges and universities that announced a major shift to remote learning canceling all in-person classes and, in some cases, asking students not to remain on campus. The trend of closing campus buildings, academic buildings, and dorms, sending students home, converting to on-line learning continues nationwide.
Click on this link for a March 2020 article regarding school shutdowns.
Click on this link to access an early March 2020 article listing colleges and universities that closed campuses and in-person classes due to the pandemic.


Pandemic Causes College Campuses To Close
By this date, 1,102 colleges and universities had closed their campuses, converting students to remote learning. It is estimated that these closures had impacted over 14 million students.
While initially thought to be a short-term closure over an extended Spring break with a return to campus, becomes apparent that the spread of the pandemic is worsening. College and universities decide over the coming weeks to remain in the remote learning phase for the remainder of the semester offering instruction and final exams on-line.
Many colleges and universities utilize software programs such as Zoom, Google Meets, and Microsoft Teams to engage students in on-line learning.
Respiratory therapist programs housed in colleges and universities nationwide are also subjected to the closures and the move to remote learning. Programs undergo pivotal changes as they work to continue instruction in the on-line environment. Many programs are forced to move not only didactic instruction, but also laboratory and clinical courses to the on-line learning arena. This requires a creative focus in providing content and instruction in ways that don’t hinder learning or negatively impact the learning process.
In early March 2020, guidance provided by the United States Department of Education (USDE) allows accrediting agencies some flexibility in addressing these circumstances. Accordingly, if face-to-face instruction and learning activities are disrupted by campus closures, distance education may be utilized to continue instruction and learning activities. CoARC allows for the need of additional time to complete programmatic accreditation requirements (for example, self-study reports, progress reports, etc.). CoARC suspends all scheduled site visits through May 15th, 2020. If needed, CoARC allows the program to consider make up options should students miss clinical time or utilize alternate sites if clinical facilities are unable to accept students due to COVID19.
While initially thought to be a short-term closure over an extended Spring break with a return to campus, becomes apparent that the spread of the pandemic is worsening. College and universities decide over the coming weeks to remain in the remote learning phase for the remainder of the semester offering instruction and final exams on-line.
Many colleges and universities utilize software programs such as Zoom, Google Meets, and Microsoft Teams to engage students in on-line learning.
Respiratory therapist programs housed in colleges and universities nationwide are also subjected to the closures and the move to remote learning. Programs undergo pivotal changes as they work to continue instruction in the on-line environment. Many programs are forced to move not only didactic instruction, but also laboratory and clinical courses to the on-line learning arena. This requires a creative focus in providing content and instruction in ways that don’t hinder learning or negatively impact the learning process.
In early March 2020, guidance provided by the United States Department of Education (USDE) allows accrediting agencies some flexibility in addressing these circumstances. Accordingly, if face-to-face instruction and learning activities are disrupted by campus closures, distance education may be utilized to continue instruction and learning activities. CoARC allows for the need of additional time to complete programmatic accreditation requirements (for example, self-study reports, progress reports, etc.). CoARC suspends all scheduled site visits through May 15th, 2020. If needed, CoARC allows the program to consider make up options should students miss clinical time or utilize alternate sites if clinical facilities are unable to accept students due to COVID19.
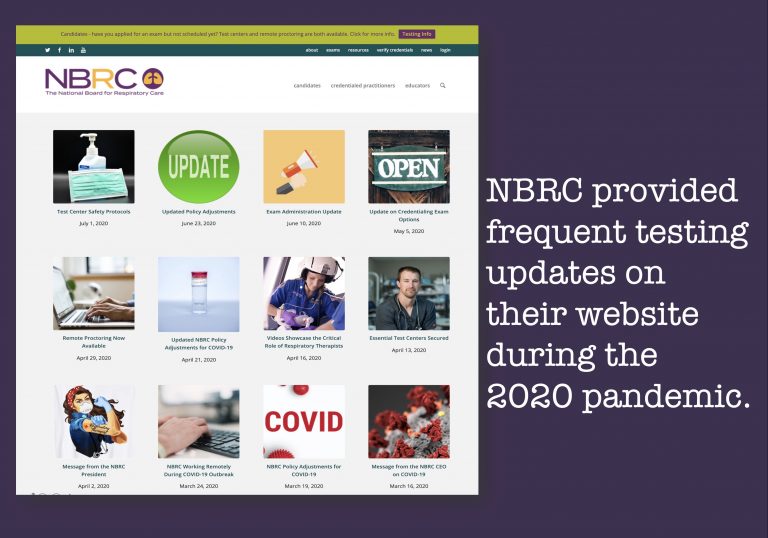

Pandemic Changes to NBRC Testing
On March 19, 2020, PSI (the test administration agency for the NBRC) closed all testing facilities.
Because of the need for respiratory therapists as essential health care workers, the NBRC secured nearly 70 PSI assessment centers for candidates to take the Therapist Multiple-Choice (TMC) and Clinical Simulation (CSE) Examinations in mid-April.
On April 29, 2020, the NBRC announced the availability of live remote online proctoring for the Therapist Multiple-Choice Examination (TMC) and Clinical Simulation (CSE) credentialing examinations.
Updates to the NBRC's testing procedures during the pandemic are available on the NBRC's website (www.nbrc.org).
Because of the need for respiratory therapists as essential health care workers, the NBRC secured nearly 70 PSI assessment centers for candidates to take the Therapist Multiple-Choice (TMC) and Clinical Simulation (CSE) Examinations in mid-April.
On April 29, 2020, the NBRC announced the availability of live remote online proctoring for the Therapist Multiple-Choice Examination (TMC) and Clinical Simulation (CSE) credentialing examinations.
Updates to the NBRC's testing procedures during the pandemic are available on the NBRC's website (www.nbrc.org).
Call to Action
On March 21, 2020, Illinois Governor JB Pritzker was one of the first governors to ask recent health care retirees to return to work during the surge in cases during the pandemic.
Respiratory therapists whose licenses had been inactive for less than five years were allowed to temporarily restore their licenses with fees and CEU requirements waived in order to return to work during the pandemic.
Click on this link to read more on the call to action.
Click on this link for a related March 24, 2020 article that discusses the initial response from healthcare workers.
Respiratory therapists whose licenses had been inactive for less than five years were allowed to temporarily restore their licenses with fees and CEU requirements waived in order to return to work during the pandemic.
Click on this link to read more on the call to action.
Click on this link for a related March 24, 2020 article that discusses the initial response from healthcare workers.

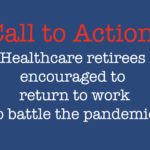
Predicted RT Shortage
A shortage of Respiratory Therapists was predicted in five states in the April 6, 2020 report from George Washington University's Milken Institute of Public Health.


Back to Our Roots
When the demand for ventilators and oxygen peaked due to the surge in COVID-19 cases, oxygen cylinders were sometimes required to meet the needs of patients housed in non-conventional sites within the hospital where piped in oxygen was not available.
A respiratory therapist from Presbyterian Brooklyn Methodist Hospital in New York City is shown in this photo along with an early inhalation therapist. Deja vu?
A respiratory therapist from Presbyterian Brooklyn Methodist Hospital in New York City is shown in this photo along with an early inhalation therapist. Deja vu?
2020 image from Felix Khusid


Dermal Injuries from PPE
During the COVID-19 pandemic, front line workers reported a variety of dermal injuries from their PPE. This April 2, 2020 post on "Tea with MD" featured a collage of PPE-related injuries.


Shortages During COVID-19 Pandemic
Due to hoarding, increased demand, and supply chain disruptions, the COVID-19 pandemic brought with it shortages of goods and supplies. These shortages to the general public included toilet paper, meat, hand sanitizer, paper towels, and cleaning supplies.
Increased patient volume in the hospital, ICU, and those requiring mechanical ventilation, led to other health care related shortages, including PPE, ventilators and requisite supplies, and respiratory therapists to care for the mechanically-ventilated patient.
To read an April 30, 2020 article from the New England Journal of Medicine about shortages of critical equipment, click on this link.
Click on this link for an April 23, 2020 article that discusses the shortages during the pandemic, including suction catheters.
Increased patient volume in the hospital, ICU, and those requiring mechanical ventilation, led to other health care related shortages, including PPE, ventilators and requisite supplies, and respiratory therapists to care for the mechanically-ventilated patient.
To read an April 30, 2020 article from the New England Journal of Medicine about shortages of critical equipment, click on this link.
Click on this link for an April 23, 2020 article that discusses the shortages during the pandemic, including suction catheters.


PPE Shortages
One solution to the shortage of N95 masks was the re-sterilization and reuse of masks. N95 masks were worn multiple shifts and at some hospitals were processed with aerosolized hydrogen peroxide for conservation of PPE supplies.
Creative individuals began supplying frontline workers with home-made shields and masks.
Click on this link for a May 29, 2020 article that features an individual who created 10,000 face shields.
Creative individuals began supplying frontline workers with home-made shields and masks.
Click on this link for a May 29, 2020 article that features an individual who created 10,000 face shields.


Sewing Guilds Upgrade Masks
An innovative local sewing guild in Peoria, Illinois upgraded over 52,000 N95 masks.
Click on this link to access the April 25, 2020 article.
Click on this link to access the April 25, 2020 article.
Image from Peoria Journal Star article April 25, 2020

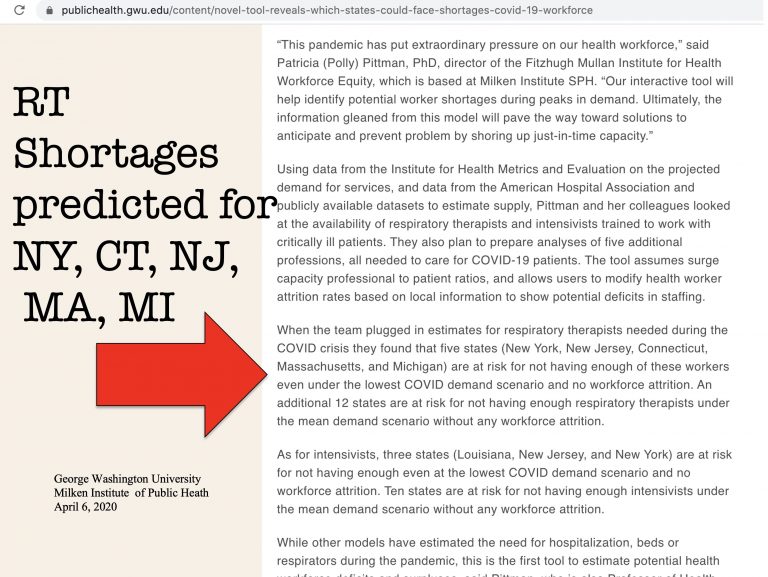
John Deere Manufactures Face Shields
The John Deere Seeding Group plant in Moline, Illinois produced and distributed over 400,000 face shields.
Click on this link to access the June 22, 2020 article.
Click on this link to access the June 22, 2020 article.
Image from June 22, 2020 QCOnline article
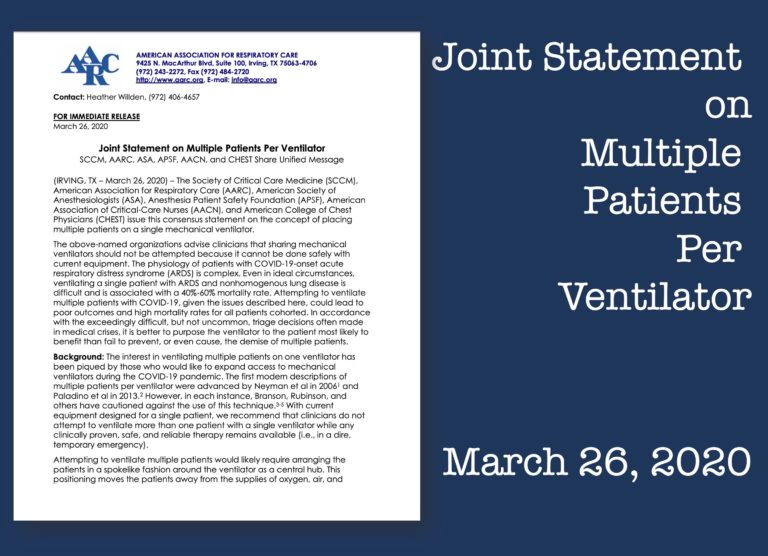
Joint Statement on Multiple Patients per Ventilator
As it was becoming apparent that the increased demand for ventilators could outstrip the supply, there were many reports and discussions about the possibility of using one ventilator for multiple patients.
Click on this link for a LiveScience article that discusses ventilator-sharing of up to 4 patients per ventilator.
Not long after these discussions, it became apparent that this practice shouldn’t be endorsed because it couldn’t be done safely with current equipment and technology. A joint statement was issued by the Society of Critical Care Medicine (SCCM), American Association for Respiratory Care (AARC), American Society of Anesthesiologists (ASA), Anesthesia Patient Safety Foundation (APSF), American Association of Critical‐Care Nurses (AACN), and American College of Chest Physicians (CHEST) discouraging this practice.
Click on this link to access the March 26, 2020 Joint Statement.
Click on this link for a LiveScience article that discusses ventilator-sharing of up to 4 patients per ventilator.
Not long after these discussions, it became apparent that this practice shouldn’t be endorsed because it couldn’t be done safely with current equipment and technology. A joint statement was issued by the Society of Critical Care Medicine (SCCM), American Association for Respiratory Care (AARC), American Society of Anesthesiologists (ASA), Anesthesia Patient Safety Foundation (APSF), American Association of Critical‐Care Nurses (AACN), and American College of Chest Physicians (CHEST) discouraging this practice.
Click on this link to access the March 26, 2020 Joint Statement.
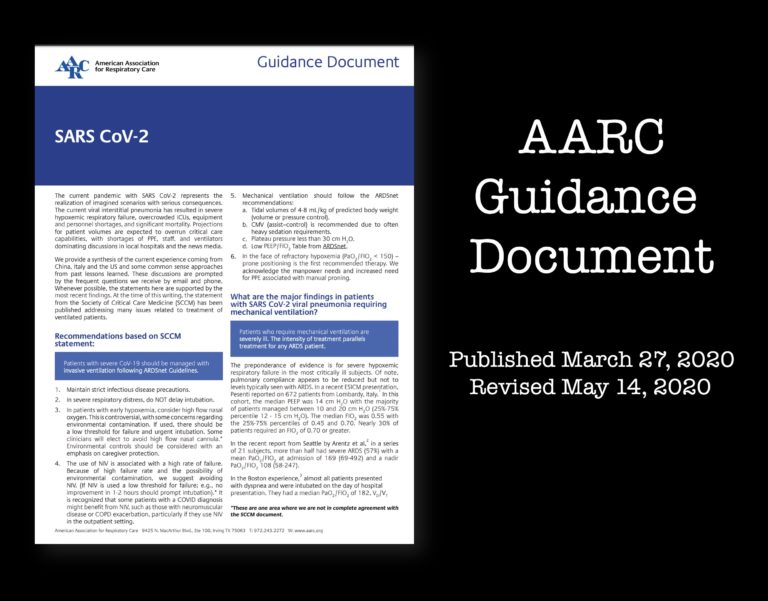
AARC Guidance Document
The AARC issued guidance on the care of patients based from past experiences and research in caring for other patients affected by ARDS in the care of patients with COVID-19.
These included concepts such as:
1. Patients with severe CoV-19 should be managed with invasive ventilation following ARDSnet Guidelines. 2. Patients who require mechanical ventilation are severely ill. 3. The intensity of treatment parallels treatment for any ARDS patient. 4. Prone position should be considered with refractory hypoxemia. 5. A heat and moisture exchanging filter (HMEF) or heated humidifier can be used in these subjects.
These included concepts such as:
1. Patients with severe CoV-19 should be managed with invasive ventilation following ARDSnet Guidelines. 2. Patients who require mechanical ventilation are severely ill. 3. The intensity of treatment parallels treatment for any ARDS patient. 4. Prone position should be considered with refractory hypoxemia. 5. A heat and moisture exchanging filter (HMEF) or heated humidifier can be used in these subjects.


Industry and Corporate America's Response
Fearing a nationwide shortage of mechanical ventilators, industry responded by increasing production of ventilators and ventilator parts.
Click on this link to read an April 12, 2020 article about Percussionaire's increased ventilator production during the pandemic.
Click on this link to read about an Ohio factory that is manufacturing ventilator components during the pandemic.
In addition, industries not previously manufacturing mechanical ventilators responded by producing ventilators for the first time ever to try and meet the anticipated need. This included mechanical ventilator production by auto companies and universities.
Click on this link to read an April 12, 2020 article about Percussionaire's increased ventilator production during the pandemic.
Click on this link to read about an Ohio factory that is manufacturing ventilator components during the pandemic.
In addition, industries not previously manufacturing mechanical ventilators responded by producing ventilators for the first time ever to try and meet the anticipated need. This included mechanical ventilator production by auto companies and universities.

Illinois RapidVent
A team led by the University of Illinois at Urbana-Champaign’s Grainger College of Engineering and Carle Health produced a prototype emergency ventilator to help address the expected surge in the need for respiratory care associated with the COVID-19 pandemic. The team worked around the clock and produced the prototype within one week.
To learn more about the RaidVent prototype, click on this link.
To learn more about the RaidVent prototype, click on this link.


Ford to Produce 50,000 Vents
On March 30, 2020, Ford Motor Corporation and GE Healthcare announced their plan to produce 50,000 ventilators in the next 100 days.
Click on this link to access the article.
Click on this link to access the article.


Vents From Car Parts
On April 6, 2020, Tesla announced their plans to create ventilators from repurposed car parts.
Click on this link to access the article.
Click on this link to access the article.


In the News
With the increased media attention on the global pandemic and its impact on the healthcare industry, respiratory therapists gained national recognition for their front-line efforts in caring for these patients. The general public finally had a basic understanding of the important role of respiratory therapists in the critical care setting.
Respiratory therapists were featured in a number of articles and newscasts during the pandemic. Click here to see a listing of interviews with AARC staff and AARC members.
Respiratory therapists were featured in a number of articles and newscasts during the pandemic. Click here to see a listing of interviews with AARC staff and AARC members.

Honoring RTs
Respiratory Therapists were honored for their work during the pandemic in this article on April 1, 2020 on Fox 24 in Fayetteville, Arkansas.
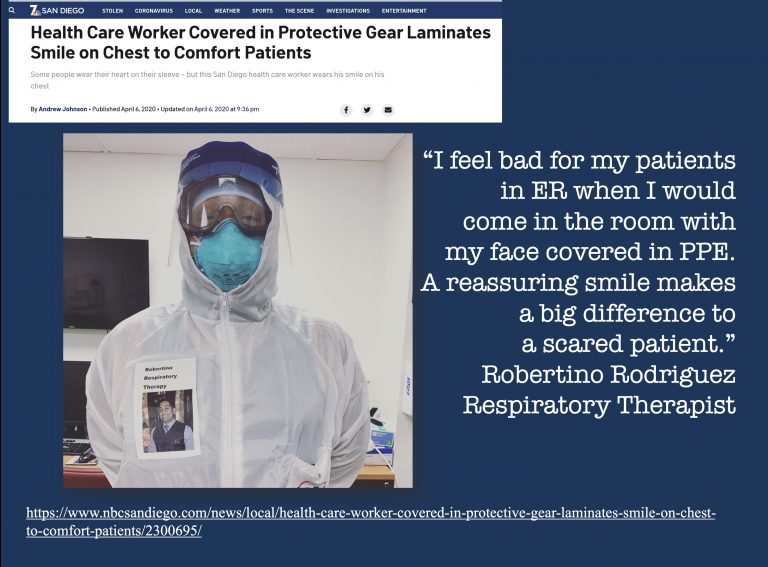

His Smile Is On His Chest
Face mask, face shield, goggles, isolation gown and gloves. This is just the start to the barrier between medical workers and patients diagnosed with COVID-19. And while these materials are imperative to ensure the safety of everyone involved, it can be quite scary for patients to never really see the people treating them.
That’s why one respiratory therapist made a special name tag to spread some comfort and joy. Robertino Rodriguez works at Scripps Mercy Hospital in San Diego, California. He puts on his personal protective equipment, known as PPE, like any other health care professional – except on the outside of his isolation gown is a special laminated badge.
"I felt bad for my patients in ER when I would come in the room with my face covered in PPE. A reassuring smile makes a big difference to a scared patient," Rodriguez wrote in an Instagram post. His giant badge lists his first name and job title in big, bold letters. And underneath, is a smiling picture of the respiratory therapist. "So my patients can see a reassuring and comforting smile," he continued.
Rodriguez posted a picture of the get-up to his Instagram page, amassing more than 10,000 likes in just two days. More than 1,000 users also commented, writing thank yous, well wishes and many, many heart emojis.
Since the outbreak began, there has been more than 1,400 COVID-19 cases in San Diego County. Roughly 18% of those who test positive for the novel coronavirus require hospitalization, according to data released by the county in early April.
Click on this link to access the April 6, 2020 article.
That’s why one respiratory therapist made a special name tag to spread some comfort and joy. Robertino Rodriguez works at Scripps Mercy Hospital in San Diego, California. He puts on his personal protective equipment, known as PPE, like any other health care professional – except on the outside of his isolation gown is a special laminated badge.
"I felt bad for my patients in ER when I would come in the room with my face covered in PPE. A reassuring smile makes a big difference to a scared patient," Rodriguez wrote in an Instagram post. His giant badge lists his first name and job title in big, bold letters. And underneath, is a smiling picture of the respiratory therapist. "So my patients can see a reassuring and comforting smile," he continued.
Rodriguez posted a picture of the get-up to his Instagram page, amassing more than 10,000 likes in just two days. More than 1,000 users also commented, writing thank yous, well wishes and many, many heart emojis.
Since the outbreak began, there has been more than 1,400 COVID-19 cases in San Diego County. Roughly 18% of those who test positive for the novel coronavirus require hospitalization, according to data released by the county in early April.
Click on this link to access the April 6, 2020 article.
Image from NBC San Diego article published April 6, 2020
Unsung Heroes
Respiratory Therapists were deemed unsung heroes in an April 17, 2020 video on ABC 10 in Modesto, California.


Unsung Heroes
Respiratory therapists were touted in the media as “unsung heroes” on CBS 4 in Indianapolis, IN on May 1, 2020.
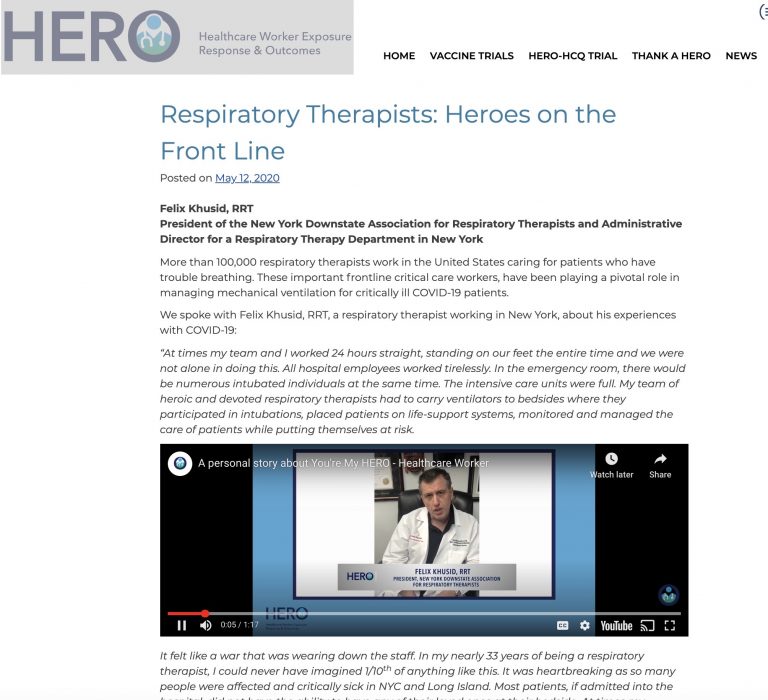

Heroes on the Front Line
Click on this link for a May 12, 2020 video featuring Felix Khusid, RRT acknowledging the dedication, support, and teamwork from all the staff working on the front lines during the pandemic.


RT Educator Shares Her Story
Kathy Rye, a respiratory therapist, survived COVID-19 after spending 46 days on a ventilator. She shared her experience in a July 8, 2020 interview.

One Million US Cases
On April 28, 2020, there were one million confirmed cases of COVID-19 reported in the United States with just over three million total cases globally.
Click on this link to read the LiveScience article.
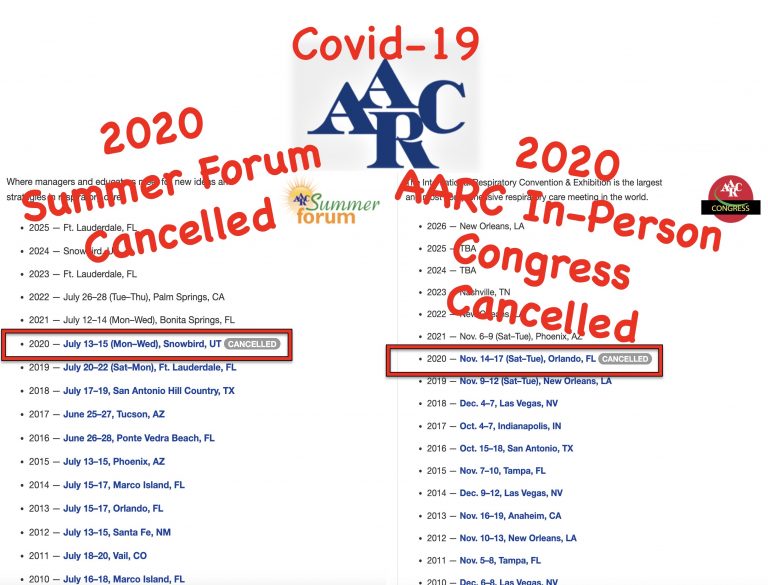

COVID-19 and the AARC
The AARC's Summer Forum was cancelled due to the pandemic.
The AARC House and Delegates and Board of Directors met virtually for their Summer meetings.
For the first time in the history of the AARC, the in-person AARC Congress was cancelled due to the pandemic. A virtual learning event, offering over 100 sessions over 4 dates in November and December 2020 will replace the traditional in-person Congress.
The AARC House and Delegates and Board of Directors met virtually for their Summer meetings.
For the first time in the history of the AARC, the in-person AARC Congress was cancelled due to the pandemic. A virtual learning event, offering over 100 sessions over 4 dates in November and December 2020 will replace the traditional in-person Congress.
5 million confirmed cases
On August 9, 2020, the media reported that the USA had reached 5 million confirmed cases of COVID-19. Over 160,000 COVID-19 deaths have been reported in the USA.
Regions of the country continue to experience upticks in confirmed cases which continues to deplete resources of equipment, supplies, and staff.
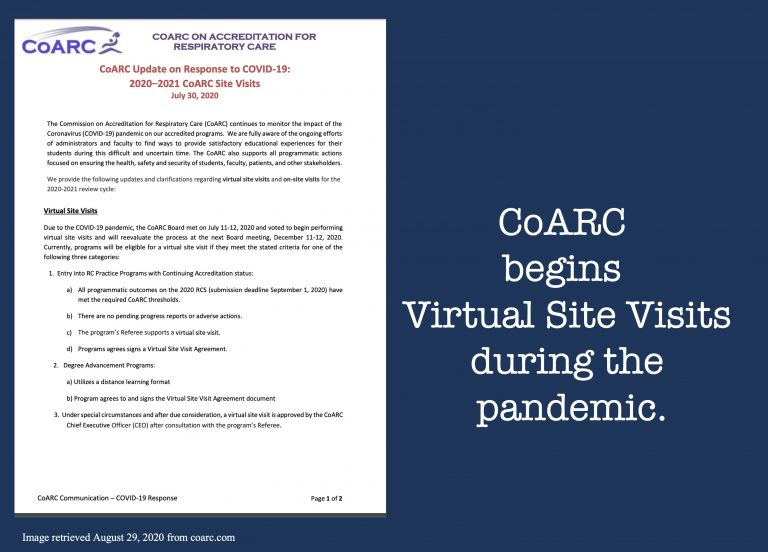
COARC Offers Virtual Site Visits
On July 30, 2020, CoARC announced they will offer the option for virtual site visits for respiratory care programs. during the pandemic.

Fall Semester Modified
Colleges and universities struggle to decide if they can reopen and if so, with what type of modifications to keep faculty, staff, and students safe from the spread of COVID-19. There are a variety of school re-opening plans with great variance. Some decide to remain on-line, while others look at modifying the academic environment to allow small group labs and discussions while delivering didactic information on-line. Many opt for a change that means students will not return to campus after Thanksgiving break at which time learning and testing will convert to on-line for the remainder of the fall semester. Most universities and colleges implement some form of testing to verify faculty, staff, and students are negative for COVID-19 and implement quarantine and self-isolation policies. Amidst a constantly changing infection rate, colleges and universities pivot with plans that change to reflect the changing infectivity rates.
Respiratory therapist programs are impacted not only by academic institutional policies, but by clinical affiliate policies related to student clinical rotations as well. The response is variable across the nation, and with infectivity rates, as well as state mandates. Programs are faced with students being unable to attend clinical sites, are restrictions on which patients/patient areas they may be allowed access to for learning purposes. Some clinical sites, for safety concerns and shortages of PPE, decide to disallow students in Emergency Departments, and COVID positive areas. Academic policies continue to evolve as the pandemic continues to progress and spread. Ultimately most instruction in most institutions moves to on-line learning, including not only didactic instruction, but lab and clinical courses being offered in an on-line format as well.
Respiratory therapist programs are impacted not only by academic institutional policies, but by clinical affiliate policies related to student clinical rotations as well. The response is variable across the nation, and with infectivity rates, as well as state mandates. Programs are faced with students being unable to attend clinical sites, are restrictions on which patients/patient areas they may be allowed access to for learning purposes. Some clinical sites, for safety concerns and shortages of PPE, decide to disallow students in Emergency Departments, and COVID positive areas. Academic policies continue to evolve as the pandemic continues to progress and spread. Ultimately most instruction in most institutions moves to on-line learning, including not only didactic instruction, but lab and clinical courses being offered in an on-line format as well.
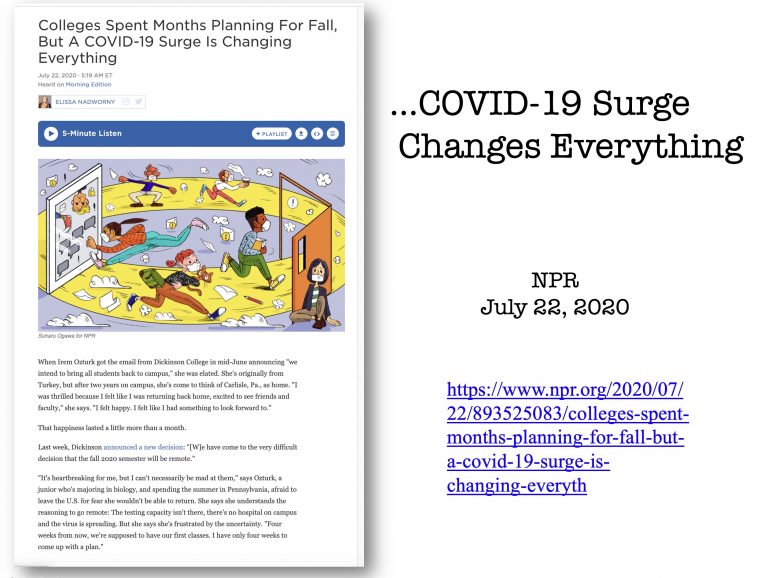
Surge Changes College Plans
Many colleges and universities announced plans to open campuses for the Fall semester only to have to modify plans due to surges in COVID-19 cases in their communities.
Some switched to remote learning for the entire semester while others offered hybrid course options and revised their course formats as COVID-19 cases occurred.
Many of the traditional college activities, such as orientation programs, sporting events, concerts, fraternity and sorority activities have been cancelled for the Fall semester.
Some switched to remote learning for the entire semester while others offered hybrid course options and revised their course formats as COVID-19 cases occurred.
Many of the traditional college activities, such as orientation programs, sporting events, concerts, fraternity and sorority activities have been cancelled for the Fall semester.
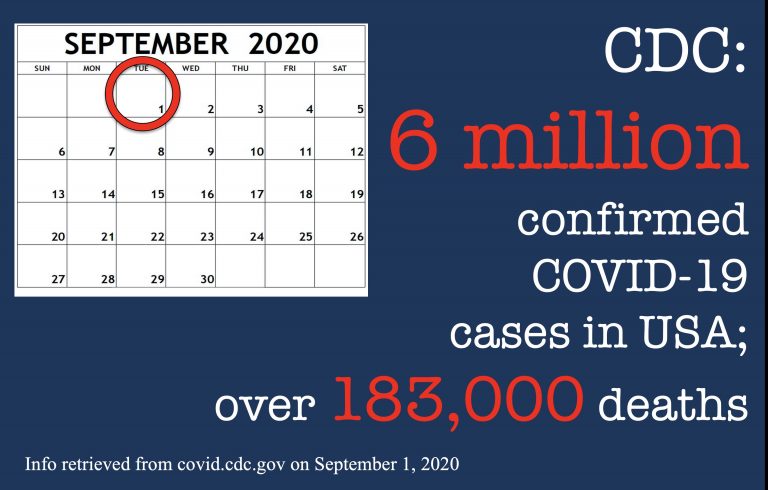
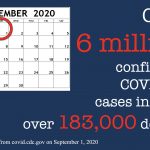
6 Million US Cases
As of September 1, 2020, the Centers for Disease Control and prevention (CDC) reported over 6 million confirmed cases of COVID-19 in the USA with over 183,000 deaths attributed to it.


200,000 Deaths in USA
On September 20, 2020, another grim milestone was reached in America: 200,000 deaths due to COVID-19.
The Bourdon Bell at the National Cathedral in Washington, DC rang 200 times on the afternoon of September 20, 2020. Each ring represented 1,000 lives lost from COVID-19.
The Bourdon Bell at the National Cathedral in Washington, DC rang 200 times on the afternoon of September 20, 2020. Each ring represented 1,000 lives lost from COVID-19.

Pandemic Fatigue
There is a weariness to continuing the practices that are put in place to help abate the spread of the virus.
As the pandemic continued without anticipated relief in positivity rates and a vaccine seemed in the distant future, exhaustion, stress, and impatience led to a feeling of overwhelmingness and hopelessness. Termed "pandemic fatigue", it identifies the sheer overwhelmingness of the pandemic in depth and breadth. Measures put in place to slow the spread of the virus, led to measures that were overwhelming—social distancing, mask wearing, limits to social gatherings, also meant isolation, depression, and a resistance to the very measures invoked to protect people from the spread of the disease.


Rapid Rise in COVID-19 Cases
Just three weeks after 7 million cases of COVID-19 were confirmed in the US, another million cases were confirmed by October 16, 2020. Another million cases had been confirmed as of October 30, 2020 reaching over 9 million cases. On November 8, 2020, 10 million cases had been confirmed. In spite of strengthened mitigation restrictions in many states, cases continued to rise and reached 11 million confirmed cases one week later.
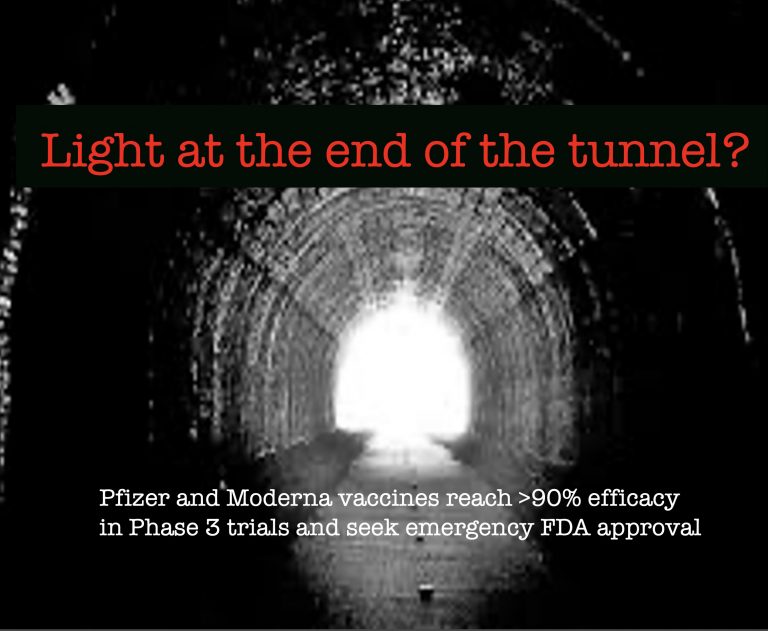
Light At The End Of The Tunnel?
During the second week of November 2020, two pharmaceutical companies reported over 90% efficacy of their COVID-19 vaccines in their Phase 3 clinical trials. Both sought emergency FDA approval.
Should the vaccines receive approval, there will still be delays while distribution plans are developed and implemented and adequate quantities of the vaccines can be made available for American citizens.
Meanwhile, for many, news of these vaccines seems like a light at the end of a long dark tunnel.
Should the vaccines receive approval, there will still be delays while distribution plans are developed and implemented and adequate quantities of the vaccines can be made available for American citizens.
Meanwhile, for many, news of these vaccines seems like a light at the end of a long dark tunnel.

Grim Milestone
On November 18, 2020, the US reached another grim milestone: 250,000 Americans have died from COVID-19 this year.
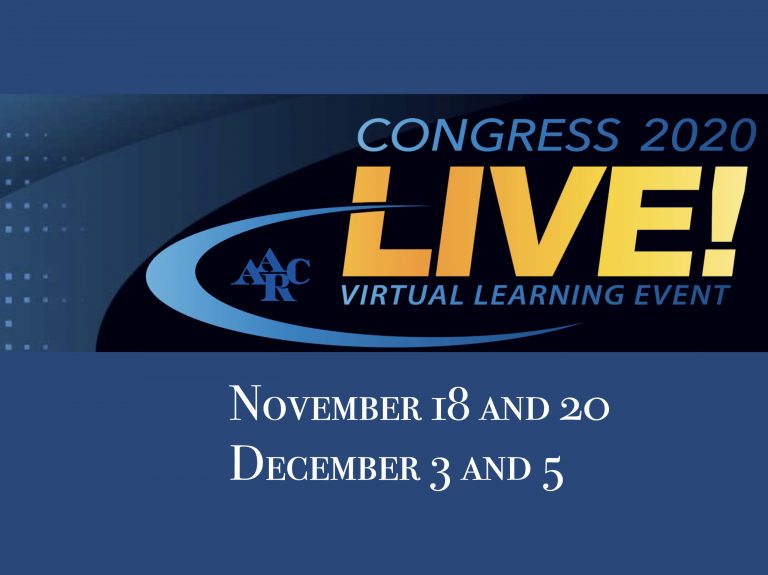
AARC Congress 2020
The AARC's 2020 Congress presentations were scheduled over four days in November and December.
The Congress presentations were recorded in advance with presenters available by Zoom to answer attendees questions. Open Forum presentations, a virtual Exhibit Hall, industry sponsored symposia, and other special activities were offered during the Congress.
The Congress presentations were recorded in advance with presenters available by Zoom to answer attendees questions. Open Forum presentations, a virtual Exhibit Hall, industry sponsored symposia, and other special activities were offered during the Congress.
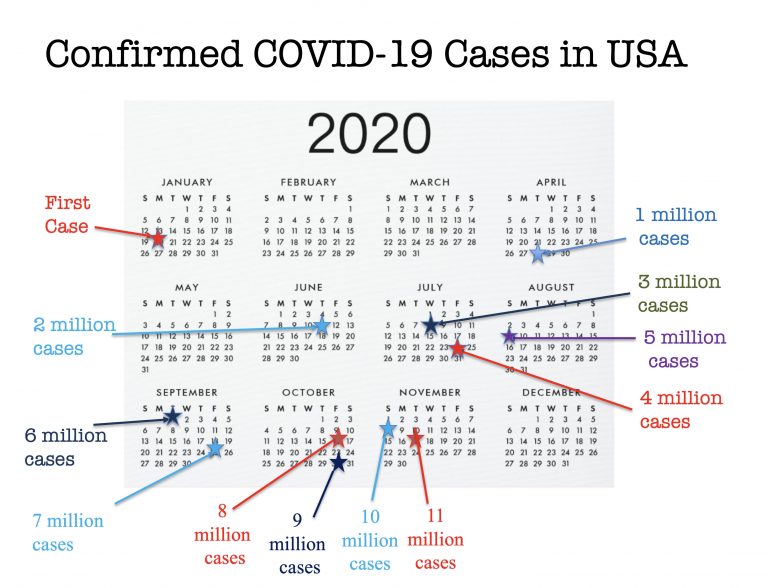
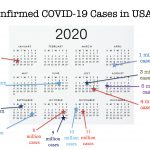
COVID-19 Case Milestones
This image summarizes the increase in COVID-19 cases in the USA from the first confirmed case on January 20, 2020
to November 17, 2020 when over 11 million cases had been confirmed.

In Memory
In appreciation of the sacrifice of the licensed respiratory therapists who died while caring for COVID-19 patients, the AARC Board of Directors authorized $500.00 to be made available to the surviving families. As of November 15, 2020, the AARC was aware of 23 respiratory therapists who have been lost during the pandemic.
The American Respiratory Care Foundation (ARCF) donated two commemorative blocks in our Wall of Donors for each of the respiratory therapists lost to COVID-19, one block for the family and one block for the employer of these RTs. Click on the DONORS icon on the museum's navigation bar then click on BLOCK DONORS to view the memorials.
The American Respiratory Care Foundation (ARCF) donated two commemorative blocks in our Wall of Donors for each of the respiratory therapists lost to COVID-19, one block for the family and one block for the employer of these RTs. Click on the DONORS icon on the museum's navigation bar then click on BLOCK DONORS to view the memorials.

Contact Us
If you have images to share for this gallery, please contact us.